Hormonal imbalance affects millions of women, causing fatigue, mood swings, irregular cycles, and fertility challenges. The good news is that natural supplements offer real support for restoring balance without the side effects of synthetic hormones.
At NuMed DPC, we’ve seen firsthand how the best natural supplements to balance female hormones can transform women’s health when combined with lifestyle changes. This guide walks you through proven options and practical strategies to reclaim hormonal stability.
Understanding Female Hormone Imbalance
What Does Hormonal Imbalance Actually Look Like
Hormonal imbalance manifests differently for every woman, but certain patterns emerge consistently. Fatigue that doesn’t improve with rest, mood swings that disrupt relationships, irregular periods that make planning impossible, unexplained weight gain around the belly, low libido, brain fog, brittle hair, and dull skin signal that your hormones need attention. A 2025 study published in Nutrients found that red meat consumption was the strongest dietary predictor of menopause timing with a 34.5% model gain, followed by BMI at 28.7%, suggesting that hormonal timing and balance are deeply influenced by what you eat and weigh. Beyond menopause, hormonal disruption stems from pregnancy and postpartum transitions, perimenopause, polycystic ovary syndrome (PCOS), endometriosis, adrenal fatigue, hypothyroidism, poor sleep, chronic stress, inadequate nutrition, and toxin exposure. More than 50 hormones influence sleep, thinking, movement, and mood, so true hormonal balance requires supporting your entire endocrine system, not fixating on a single hormone. This explains why women often experience a cascade of symptoms rather than isolated issues.
Why Supplements Alone Won’t Fix the Problem
Natural supplements work best when they address root causes rather than mask symptoms. The UK Women’s Cohort Study, which tracked 3,566 women, found that supplement users reached menopause at a median age of 51 years compared to 50 years for non-users-a meaningful but modest difference.
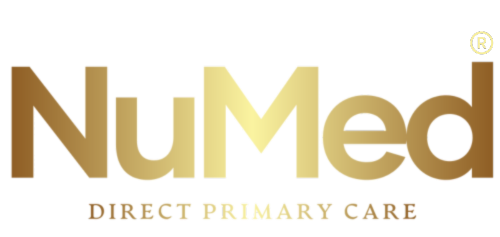
What mattered more was the overall dietary pattern. The research showed that omega-3 fatty acids from fish oil were linked to a 95% lower hazard of earlier menopause, vitamin B-complex to a 52% lower hazard, and antioxidant combinations to a 46% lower hazard. However, multivitamin-multimineral formulations showed no significant effect on menopause timing, meaning generic supplement approaches fail. The evidence strongly suggests that specific, food-derived nutrients matter far more than broad-spectrum supplements. Magnesium deficiency affects up to 50% of the population, vitamin D deficiency occurs in roughly 42% of American adults, and most women consume inadequate fiber, yet supplements only work when lifestyle foundations are in place.
Building a Foundation That Supplements Can Actually Support
Supplements amplify the effects of solid fundamentals rather than replace them. Your sleep directly controls when and how hormones are produced and released through your circadian rhythm, so try for at least 7 hours nightly. Stress management matters because cortisol dysregulation cascades through your entire hormonal system, making daily stress-reduction practices essential. Nutrition shapes your hormonal destiny more than any pill. Fiber intake of 25 to 30 grams daily supports gut bacteria that regulate hormone metabolism and estrogen clearance, yet most American women fall short. Exercise at 150 minutes of moderate activity or 75 minutes of vigorous activity weekly reduces hot flashes, improves mood, and stabilizes blood sugar, which becomes critical as estrogen declines. Limiting refined carbohydrates prevents insulin spikes that disrupt estrogen balance during perimenopause and menopause. When these foundations are solid, targeted supplements like magnesium bisglycinate (350 milligrams daily), vitamin D3 (1,000 IU daily), and omega-3 fatty acids actually produce measurable improvements rather than serving as expensive urine.
How Specific Nutrients Restore Hormonal Function
The science shows that certain nutrients restore hormonal function more effectively than others. Magnesium helps calm your HPA axis, supports liver processing of hormones, and aids conversion of T4 to T3 thyroid hormone. Vitamin D acts as a hormonal precursor and deficiency directly impairs mood and bone health. Omega-3 fatty acids support brain, bone, and heart health while aiding hormone production and receptor sensitivity. Vitamin B6 supports estrogen and progesterone balance, particularly for premenstrual symptoms. Zinc converts T4 to T3, helps rebalance cortisol, estrogen, and progesterone, and reduces inflammation. These nutrients work synergistically when obtained from food sources first, then supplemented strategically when dietary intake falls short. The next section explores the top natural supplements that research supports for hormone balance and how to use them effectively.
Top Natural Supplements for Hormone Balance
Vitex: Evidence for Progesterone Support
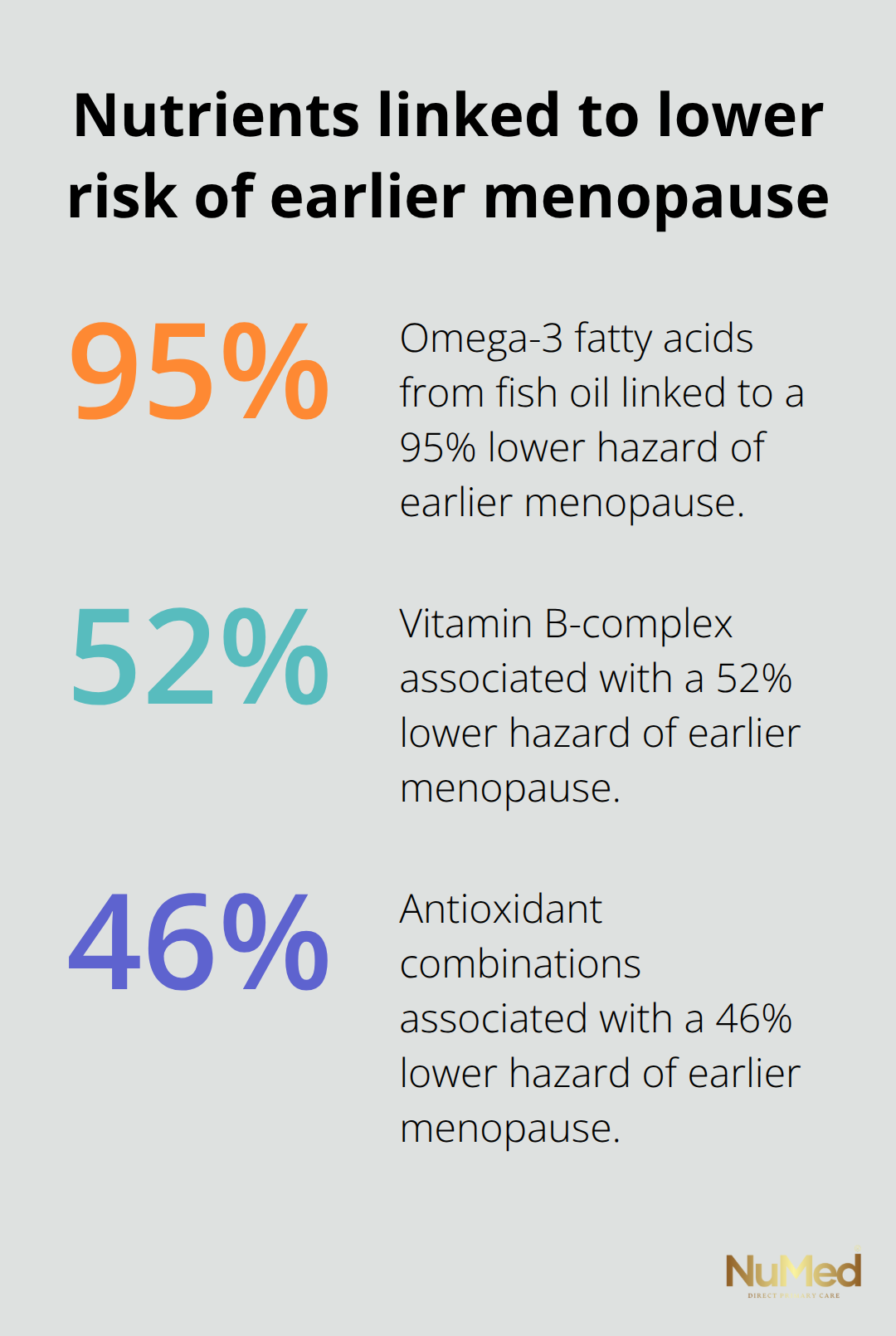
Vitex, also called chasteberry, shows the strongest evidence for progesterone support, particularly for premenstrual syndrome. A Cochrane review of randomized trials found that chasteberry reduced breast pain and tenderness in some women, though results weren’t universal across all PMS presentations. The mechanism works through vitex’s influence on luteinizing hormone, which signals your body to produce progesterone in the luteal phase. The typical dose ranges from 300 to 600 milligrams daily of standardized extract, taken consistently for at least three months to assess effectiveness. Safety data from the NIH Office of Dietary Supplements shows chasteberry is well-tolerated short-term, with mild side effects like nausea or headache occurring in a small percentage of users.
Critical caveat: chasteberry should be avoided entirely if you have hormone-sensitive breast, uterine, or ovarian cancer, and pregnancy makes it unsafe, so clinical guidance is non-negotiable before starting. Women with luteal phase symptoms should explore vitex under clinical supervision to determine whether it helps their specific presentation.
Maca Root: Limited Evidence Despite Marketing Claims
Maca root presents a different scenario because high-quality evidence remains limited despite widespread marketing claims. Studies examining maca for menopausal symptoms show inconsistent results, with some women reporting mood improvement and others experiencing no change.
The isoflavone content in maca may modestly support estrogen metabolism, but calling it an estrogen support supplement overstates current evidence. A practical dose of 1,500 to 3,000 milligrams daily appears safe in short-term studies, yet long-term safety data are sparse. Menopausal women should frankly skip maca in favor of proven lifestyle modifications and, when appropriate, bioidentical hormone therapy.
Spearmint Tea: Genuine Androgen Reduction
Spearmint tea offers the most straightforward evidence for a specific hormonal problem: elevated androgens in PCOS and hirsutism. Two randomized controlled trials found that spearmint tea daily for eight weeks showed reduced free testosterone and improved androgen-related symptoms compared to placebo. This represents genuine, replicable clinical benefit without the side effects of anti-androgen medications. The mechanism involves compounds in spearmint that inhibit certain enzymes in androgen synthesis. You can obtain spearmint tea inexpensively from any grocery store, brew it fresh, and drink it consistently without worrying about standardization issues that plague many herbal supplements. Women with PCOS benefit most from spearmint tea as a targeted intervention. The three-month commitment applies here, too, because hormonal shifts don’t happen overnight and your body needs sustained exposure to demonstrate benefits.
Supplement Quality and Selection Strategy
What separates effective supplements from expensive placebos is honest acknowledgment of evidence strength. Vitex works for some women’s PMS symptoms but not all, maca lacks compelling proof for menopause relief, and spearmint tea genuinely reduces androgens in specific conditions. None of these supplements replaces the foundational work of sleep optimization, stress management, and dietary changes that matter more. Supplement quality varies dramatically because the FDA doesn’t pre-approve herbal products before sale, meaning manufacturers control their own safety and potency claims. Select products with USP or NSF certification, which indicate third-party testing for contaminants and accurate labeling. Avoid purchasing the cheapest option because substandard extraction methods or ingredient substitution occur frequently in low-cost supplements.
Start with one supplement at a time so you can clearly identify whether it helps or causes side effects, then wait at least 12 weeks before concluding it doesn’t work. The temptation exists to combine vitex plus maca plus spearmint plus five other supplements simultaneously, but this approach obscures which ingredient actually helps you and creates unnecessary interaction risks. Lifestyle factors amplify whatever supplement support you choose, making the next chapter essential for maximizing your hormonal health outcomes.
Lifestyle Habits Control Hormone Stability
Sleep Synchronization Drives Hormonal Rhythm
Supplements fail when sleep remains broken, stress stays chronically elevated, and nutrition stays poor. Circadian rhythm controls when your body releases hormones, and disrupting it undermines every supplement you take. Most women need seven to nine hours nightly, yet the average American woman sleeps 6.8 hours, creating a cumulative hormone deficit. Poor sleep directly impairs progesterone production, elevates cortisol, and increases insulin resistance, which accelerates perimenopause symptoms and weight gain.
Consistency matters more than the exact hour you choose. A consistent sleep schedule nightly produces better hormonal outcomes than sleeping variable hours, even if total hours match, because your body synchronizes hormone production to your schedule. Track your sleep for two weeks and identify your actual pattern rather than guessing. If you average 6.5 hours, add 30 minutes nightly until you reach seven hours minimum, then assess whether fatigue, mood, and cycle regularity improve. This typically takes four to six weeks because your hormonal system recalibrates slowly.
Stress Management Restores Cortisol Balance
Cortisol dysregulation amplifies every other hormonal problem because elevated cortisol suppresses progesterone, increases belly fat storage, and disrupts thyroid function. Chronic stress doesn’t require a dramatic life event; daily frustration, work deadlines, and relationship tension accumulate into sustained cortisol elevation that sabotages supplement effectiveness. Carving out 15 minutes daily for stress reduction costs nothing and produces measurable hormone shifts.
Research shows that consistent stress management practices lower cortisol more reliably than expensive adaptogenic supplements, making meditation, walking, or breathing exercises your first intervention. Start with ten minutes of focused breathing daily for two weeks and track whether sleep quality, anxiety, or cycle symptoms improve before adding supplements.
Protein and Fiber Build Hormonal Foundation
Nutrition shapes hormone production more directly than any pill because your body builds hormones from dietary components. Adequate protein intake matters because amino acids form the backbone of hormones themselves; women need 0.8 to 1.0 grams per kilogram of body weight daily, meaning a 150-pound woman requires roughly 55 to 68 grams daily. Most women undershoot this target, then wonder why their hormones remain unstable despite supplementation.
Fiber intake of 25 to 30 grams daily supports the gut bacteria that metabolize estrogen and clear excess hormones, yet the average American woman consumes 15 grams. This single deficit explains why so many women experience prolonged perimenopause despite taking vitex or maca. Add fiber gradually through whole grains, legumes, and vegetables because rapid increases cause bloating that feels worse than the original imbalance.
Dietary Patterns Predict Hormonal Timing
Red meat consumption predicted menopause timing more strongly than any other dietary factor in the 2025 Nutrients study, suggesting that limiting red meat to two servings weekly while prioritizing fish, poultry, and plant-based proteins supports hormonal stability. Fish provides omega-3 fatty acids that reduce ovarian inflammation and support hormone receptor sensitivity, making fatty fish two to three times weekly a genuine intervention rather than optional.
Exercise Stabilizes Hormones Without Supplements
Exercise reduces hot flashes, stabilizes blood sugar, and improves mood through mechanisms independent of supplements. Try 150 minutes of moderate activity or 75 minutes of vigorous activity weekly, split into sessions you’ll actually maintain rather than ambitious goals you’ll abandon.
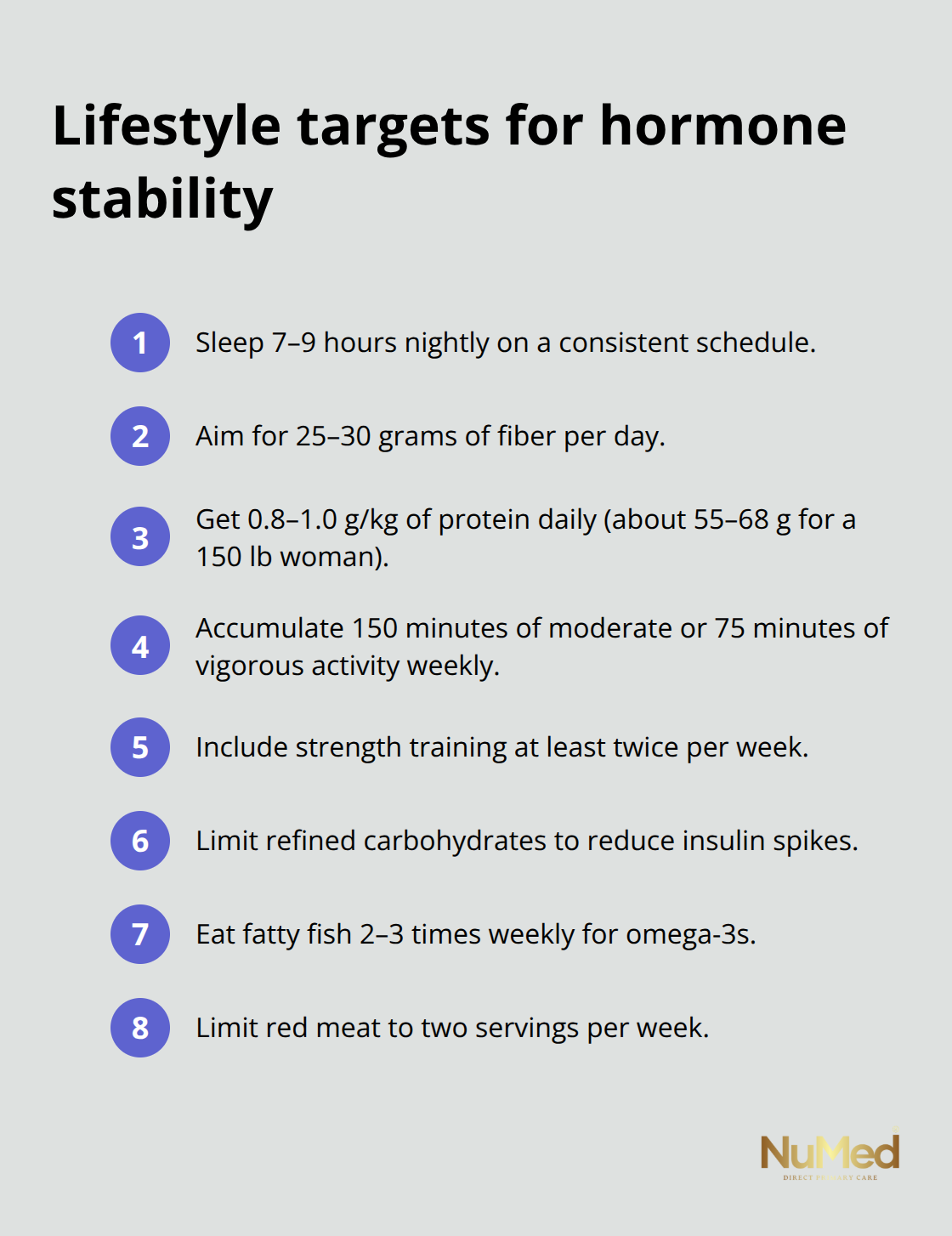
Strength training twice weekly matters more than additional cardio because muscle tissue improves insulin sensitivity and metabolic flexibility, both critical as estrogen declines (walking counts as moderate activity, so this doesn’t require gym membership or expensive equipment).
Start with your actual current activity level, then add ten minutes weekly until you reach 150 minutes. This progression prevents injury and builds habit sustainability that supplements can’t provide alone.
Final Thoughts
The best natural supplements to balance female hormones only work when you build a solid foundation with sleep, stress management, nutrition, and exercise. Vitex reduces PMS symptoms for some women, spearmint tea genuinely reduces androgens in PCOS, and maca root lacks compelling evidence despite marketing claims. These distinctions matter because honest assessment prevents wasting money on supplements that won’t help your specific situation.
Your hormonal system responds to patterns, not isolated interventions. A woman who takes vitex while sleeping six hours nightly, eating processed foods, and managing chronic stress will see minimal improvement, whereas the same woman prioritizing seven hours of sleep, eating adequate protein and fiber, moving her body regularly, and taking vitex will likely experience meaningful shifts within three months. This explains why supplement effectiveness varies so dramatically between women-the supplement isn’t the variable that changes outcomes.
Personalization matters because hormonal imbalance stems from different root causes in different women (PCOS requires androgen reduction through spearmint tea and dietary changes, perimenopause requires progesterone support through vitex and lifestyle optimization, and postmenopause requires bone health support through exercise and adequate calcium and vitamin D). Start by tracking your actual sleep, stress, nutrition, and exercise patterns for two weeks, then add one targeted supplement while maintaining consistent lifestyle practices. If symptoms persist despite these efforts, seek care from a clinician who specializes in women’s hormonal health for a tailored plan that addresses your specific situation.