Hormonal fluctuations affect nearly every woman at some point in her life, influencing energy, mood, metabolism, and overall health. At NuMed DPC, we believe understanding how natural hormones work is the first step toward reclaiming your wellness.
This guide walks you through the science behind female hormones, practical strategies to support balance naturally, and when bioidentical options might be right for you.
Understanding Female Hormones and Their Functions
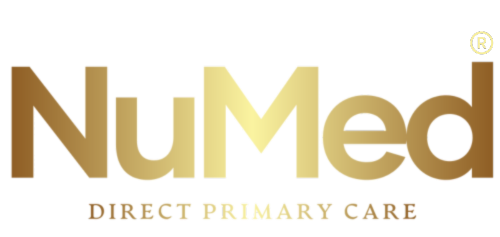
How Your Three Key Hormones Shape Your Health
Estrogen, progesterone, and testosterone regulate your menstrual cycle, bone density, cardiovascular function, and mood. Estrogen drives the proliferation of the uterine lining during the follicular phase of your cycle, typically rising from 25 to 400 picograms per milliliter as you approach ovulation. Progesterone rises sharply after ovulation, peaking at 10 to 20 nanograms per milliliter, and this hormone maintains the uterine lining, supports pregnancy, and promotes sleep quality. Testosterone, though produced in smaller amounts in women than men, plays a critical role in bone strength, muscle maintenance, and sexual desire, with healthy levels ranging from 15 to 70 nanograms per deciliter. When these three hormones work in balance throughout your cycle, your body functions optimally. When they fall out of sync, the effects ripple across your entire system.
What Happens When Hormones Fall Out of Balance
Hormonal imbalance in women creates cascading health problems that extend far beyond reproductive health. Excess estrogen relative to progesterone-a condition called estrogen dominance, causes heavy periods, breast tenderness, weight gain in the hips and thighs, and increased anxiety. Low progesterone impairs your ability to sleep deeply and reduces your capacity to manage stress effectively because progesterone activates GABA receptors in your brain, which calms nervous system activity. Insufficient testosterone weakens your bones, reduces your muscle mass, and diminishes your libido and sense of well-being. Declining estrogen during perimenopause and menopause triggers hot flashes, vaginal dryness, mood swings, and accelerated bone loss. These hormonal shifts create widespread effects across your body systems.
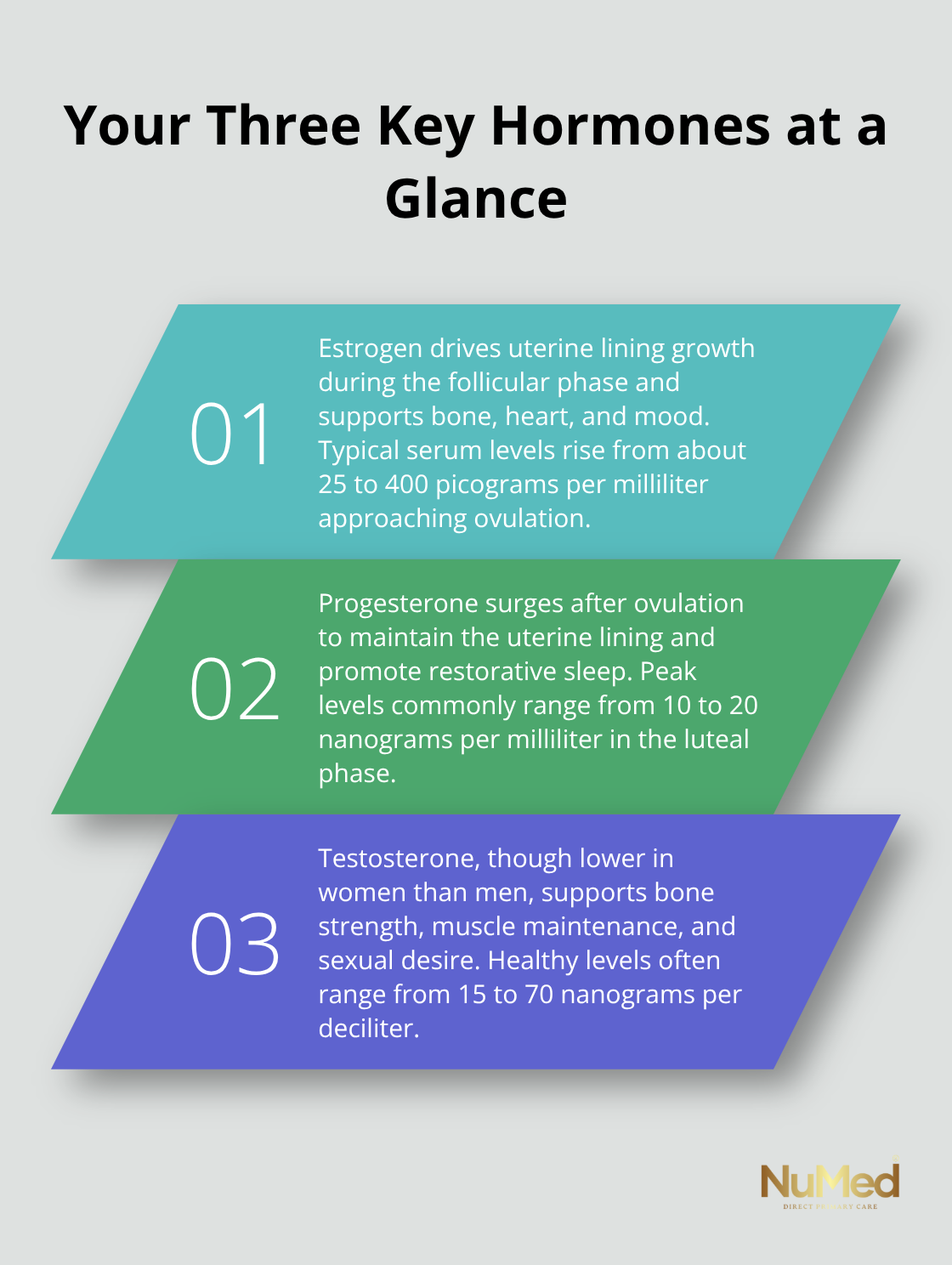
Recognizing the Signs Your Hormones Need Attention
The symptoms of hormonal disruption vary widely because hormones affect so many body systems simultaneously. Irregular or heavy periods, severe PMS symptoms lasting more than a week, persistent bloating, unexplained weight gain despite consistent diet and exercise, brain fog, mood swings, insomnia, low libido, and joint aches often signal that your hormones are out of range. Fatigue that doesn’t improve with sleep, hair loss or thinning, dry skin, and temperature regulation problems (whether you’re freezing when others are comfortable or constantly overheating) are equally important red flags.
Some women experience all of these simultaneously during perimenopause, while others notice only one or two persistent symptoms. The key is recognizing that these aren’t separate problems requiring separate treatments; they’re signals from a single system out of balance.
Moving Beyond Symptom Treatment
Most conventional approaches treat each symptom independently, prescribing sleep aids for insomnia, antidepressants for mood swings, and topical creams for dry skin. This fragmented approach misses the hormonal root cause driving your entire experience. A comprehensive assessment of your complete hormonal picture through lab work reveals which specific hormonal dysfunctions create your symptoms. Once you understand your actual hormone levels and ratios, you can address the source rather than chasing individual complaints. The next section explores the natural approaches that work with your body’s biology to restore hormonal balance.
How to Rebuild Hormonal Balance Through Food, Movement, and Targeted Supplements
Dietary Strategies That Support Hormone Metabolism
Restoring hormonal balance requires working with your body’s biology rather than against it. The foods you eat directly influence hormone production and metabolism because your liver processes and recycles estrogen through the enterohepatic circulation, making adequate fiber intake non-negotiable for hormonal health. Cruciferous vegetables like broccoli, Brussels sprouts, and cabbage contain sulforaphane, a compound that supports estrogen metabolism and helps prevent estrogen dominance. Fatty fish rich in omega-3 fatty acids reduce inflammation, which drives many hormonal imbalances. Ground flaxseeds contain lignans that bind excess estrogen in your digestive tract, preventing reabsorption-try 1-2 tablespoons daily mixed into yogurt or smoothies.
Refined carbohydrates and seed oils spike insulin and promote inflammation, both of which disrupt progesterone production and trigger weight gain. Protein at every meal provides amino acids that build neurotransmitters regulating mood and stress response. Adequate zinc intake matters significantly for progesterone production, so include oysters, beef, pumpkin seeds, or supplemental zinc picolinate at 15-30 milligrams daily if you’re deficient.
Movement and Sleep as Hormonal Regulators
Stress management directly impacts cortisol levels, and chronically elevated cortisol suppresses progesterone production while promoting estrogen dominance, creating a vicious cycle of worsening symptoms. Resistance training 3-4 times weekly builds muscle mass, which stabilizes blood sugar and improves insulin sensitivity-both critical for hormonal balance. Consistent sleep of 7-9 hours matters because sleep deprivation increases estrogen production and reduces progesterone, explaining why perimenopausal women often experience worse symptoms when sleep suffers.
Targeted Supplementation Based on Your Actual Needs
Vitex (chasteberry) increases progesterone levels, with clinical research showing women taking 400-500 milligrams daily experienced reduced PMS severity and more regular cycles within 3 months. Magnesium glycinate at 300-400 milligrams nightly calms your nervous system and supports progesterone’s GABA activity, addressing both anxiety and sleep simultaneously. Maca root contains bioactive compounds that support libido and mood, particularly during perimenopause, with effective doses ranging from 1.5-3 grams daily. N-acetylcysteine (NAC) supports liver detoxification pathways and reduces androgens in polycystic ovary syndrome; studies show 1.8-2.4 grams daily for 12 weeks improved ovulation rates.
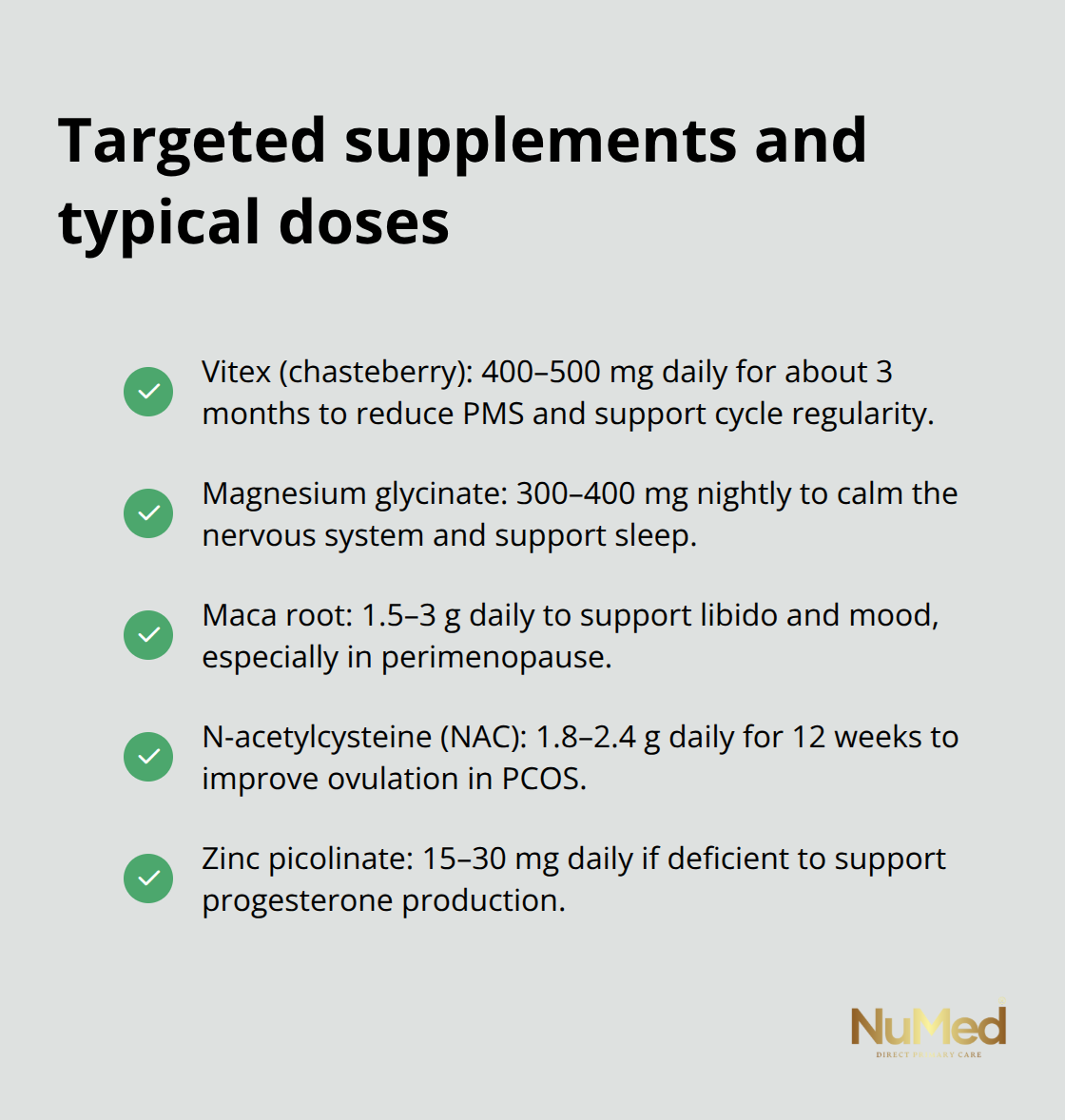
Rather than taking random supplements, get specific lab work done to identify your actual deficiencies and hormonal imbalances. This targeted approach means your supplementation strategy addresses your real problems rather than generic hormone support. Understanding your complete hormonal picture through comprehensive testing reveals which specific interventions will move the needle for your unique situation.
Bioidentical Hormones vs Synthetic: What the Research Actually Shows
How Bioidentical and Synthetic Hormones Differ
Bioidentical hormones and synthetic hormones differ fundamentally in structure, and this difference matters for how your body processes them. Bioidentical hormones match your body’s natural hormone molecules exactly-estradiol is estradiol, progesterone is progesterone-while synthetic hormones contain altered chemical structures that stay in your system longer and produce stronger effects. Premarin, a commonly prescribed synthetic estrogen, comes from pregnant mare urine and contains estrone sulfate, a form of estrogen your body doesn’t naturally produce in significant amounts. Medroxyprogesterone acetate, the synthetic progestin in Provera, differs structurally from natural progesterone and binds to progesterone receptors differently, producing side effects your body wasn’t designed to tolerate.
What the Research Reveals About Safety
The Women’s Health Initiative study published in 2002 followed 16,608 women taking conjugated equine estrogens plus medroxyprogesterone acetate and found increased rates of breast cancer, blood clots, and stroke compared to placebo. These findings sparked decades of debate about hormone therapy safety and shifted clinical practice toward more cautious approaches. Bioidentical hormones work with your existing receptor sites more naturally because they’re molecularly identical to what your ovaries produce, theoretically reducing some adverse effects, though long-term safety data remains limited compared to synthetic options.
Clinical Evidence for Bioidentical Hormone Therapy
Clinical evidence on bioidentical hormone therapy shows mixed but promising results for symptom relief without the severity of side effects associated with synthetic hormones. A 2016 systematic review in Menopause found that women using bioidentical estradiol and micronized progesterone experienced significant improvement in hot flashes and night sweats with fewer reports of breast tenderness and mood changes than those on synthetic alternatives. The key difference lies in dosing flexibility-bioidentical hormones allow customization to your individual needs through compounded formulations, letting your practitioner adjust doses based on your specific lab values and symptoms rather than forcing you into standardized doses designed for average populations.
Personalization Matters More Than One-Size-Fits-All Protocols
This personalization matters because a woman with severe hot flashes but normal bone density needs a different approach than a woman experiencing primarily vaginal dryness with declining bone markers. A practitioner who takes time to understand your individual situation rather than applying a one-size-fits-all protocol can recommend treatment that matches your actual biochemistry. The decision between bioidentical and synthetic hormones depends on your symptom severity, risk factors, personal health history, and how your body responds during an initial trial period.
Final Thoughts
Hormonal balance requires ongoing attention rather than a one-time fix. The strategies in this guide work because they address the actual mechanisms driving your symptoms instead of masking them temporarily. Natural hormones for women function best when you support them through consistent dietary choices, adequate sleep, stress management, and targeted supplementation matched to your specific needs.
Your hormonal picture is uniquely yours, and a woman experiencing estrogen dominance with severe PMS needs a completely different approach than one facing perimenopause with declining progesterone. Generic protocols fail because they ignore this fundamental truth, which is why comprehensive lab work matters-it reveals your actual hormone levels and ratios rather than forcing you into assumptions about what’s wrong. Some women restore complete balance through dietary changes and supplements within three to six months, while others need bioidentical support to reach symptom relief while their lifestyle modifications take effect.
Finding a practitioner who takes time to understand your complete health picture matters more than following any single protocol. You deserve someone who orders appropriate testing, listens to your symptoms, and customizes treatment to your needs rather than applying standardized approaches to everyone. Explore direct primary care to discover how personalized medicine and comprehensive lab services can support your hormonal wellness journey with the individualized approach your body deserves.