Mental health treatment has evolved significantly over the past century, with the medical model becoming one of the most influential frameworks in psychiatry and psychology. This approach views mental health conditions through a clinical lens, emphasizing diagnosis, assessment, and evidence-based interventions.
At NuMed DPC, we recognize that understanding the medical model mental health framework helps patients make informed decisions about their care. Whether you’re exploring treatment options or seeking clarity on how different approaches work, this overview provides the foundation you need.
What Is the Medical Model in Mental Health?
The medical model treats mental health conditions as diseases with identifiable biological origins. Rather than viewing mental illness as a moral failing or purely psychological issue, this framework positions psychiatric symptoms alongside physical symptoms-both stem from measurable brain dysfunction. Psychiatrists trained in this model focus on neurotransmitter imbalances, genetic predisposition, and neurophysiological changes that correspond to specific diagnoses. When you receive a diagnosis of major depression, anxiety disorder, or bipolar disorder under this model, clinicians identify a recognized syndrome based on symptom clusters and functional impairment, much as they would diagnose diabetes or hypertension. This approach gained prominence in the mid-twentieth century as neuroscience advanced and medications like selective serotonin reuptake inhibitors proved effective for conditions like anxiety and depression. The American Academy of Family Physicians recognizes that this medical framework remains the dominant model in psychiatric practice today, particularly among psychiatrists who emphasize pharmacological treatment alongside diagnostic clarity.
Brain Chemistry as the Foundation
The medical model rests on the assumption that correcting brain chemistry reduces symptoms. In anxiety disorders, for instance, serotonin regulation is often implicated. The theory suggests that insufficient serotonin availability in the synaptic gap contributes to worry, panic, and avoidance. SSRIs work by blocking serotonin reuptake, increasing the amount available to brain cells. This biological emphasis extends to genetics, neuroanatomy, and neurophysiology as core factors that shape mental health. The model applies disease-management logic: identify the problem through diagnostic assessment, target the underlying mechanism with medication, and monitor outcomes. Symptoms like hallucinations represent signs of organic dysfunction rather than purely psychological phenomena, which guide both diagnosis and intervention.
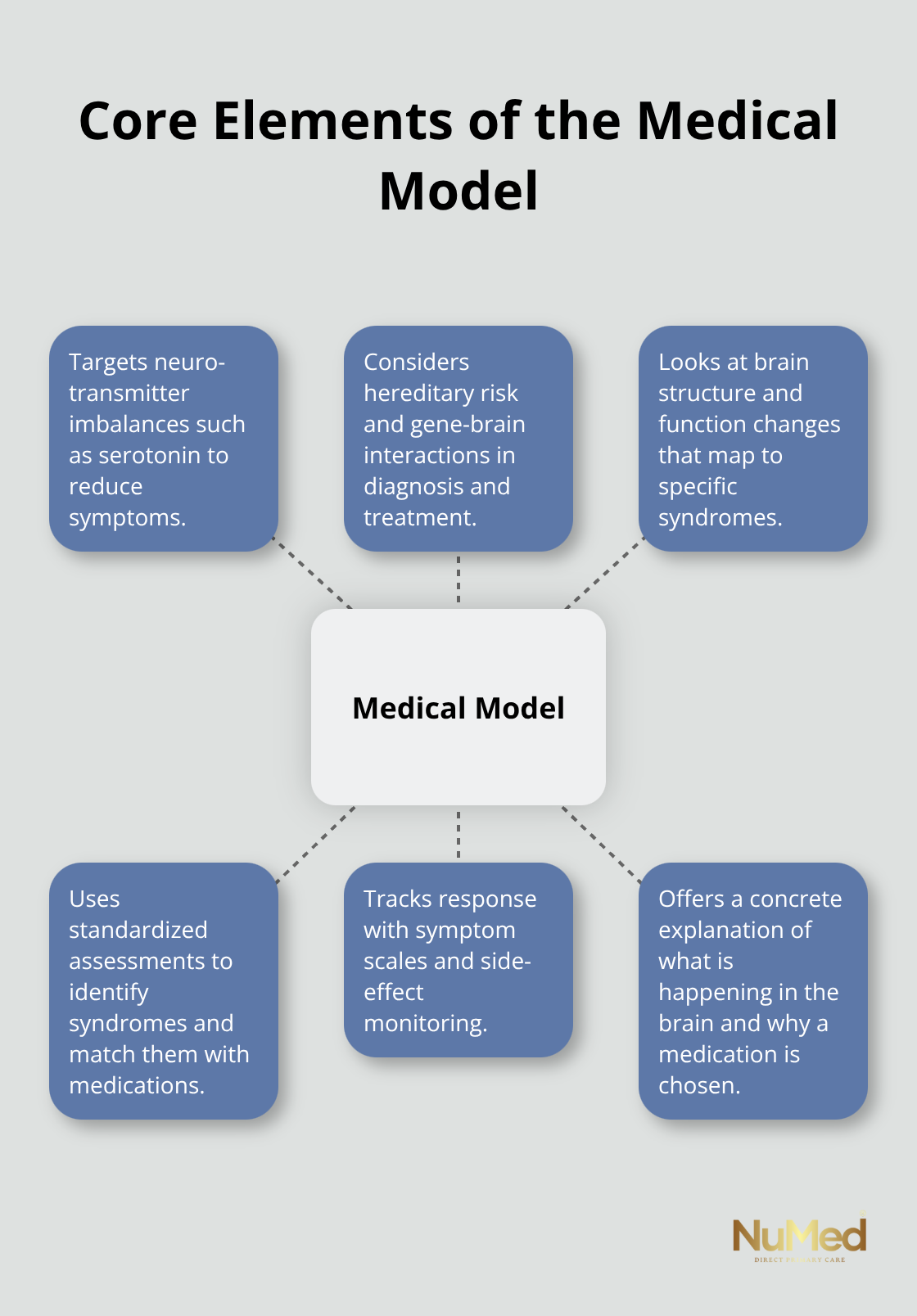
This concrete, measurable approach appeals to patients who want clarity about what happens in their brain and why specific medications are recommended.
How the Medical Model Differs from Other Approaches
The medical model differs fundamentally from social and psychological frameworks that emphasize environmental or relational factors. Social perspectives argue that oppression, poverty, discrimination, and systemic inequality contribute significantly to mental distress, suggesting that broader societal change matters as much as medication. Psychological approaches emphasize thought patterns, learned behaviors, and emotional processing, often prioritizing talk therapy over pharmacology. Many experts today advocate a biopsychosocial approach that integrates medication management with psychotherapy and psychosocial interventions, recognizing that neither biology nor environment tells the complete story. However, the medical model’s strength lies in its empirical foundation: diagnoses are syndromes based on observable symptom clusters, treatments undergo testing through peer-reviewed research, and outcomes can be measured objectively. Critics argue the model underemphasizes how life circumstances shape mental health and may lead to over-medicalization of normal human suffering.
The Role of Personalized Assessment
Effective mental health care often combines evidence-based medical assessment with functional medicine principles that address root causes. This integrated approach examines nutrition, sleep, hormones, and lifestyle factors alongside appropriate medication management when indicated. Clinicians who adopt this perspective recognize that a patient’s symptoms reflect both biological mechanisms and life context. The medical model provides the diagnostic framework and pharmacological tools, while functional and holistic perspectives add depth by investigating what drives the biological dysfunction in the first place. This combination allows practitioners to move beyond symptom suppression toward sustainable recovery. As you consider treatment options, understanding how these different frameworks complement each other helps you evaluate what approach aligns with your needs and values.
How the Medical Model Guides Diagnosis and Treatment
Structured Diagnostic Assessment
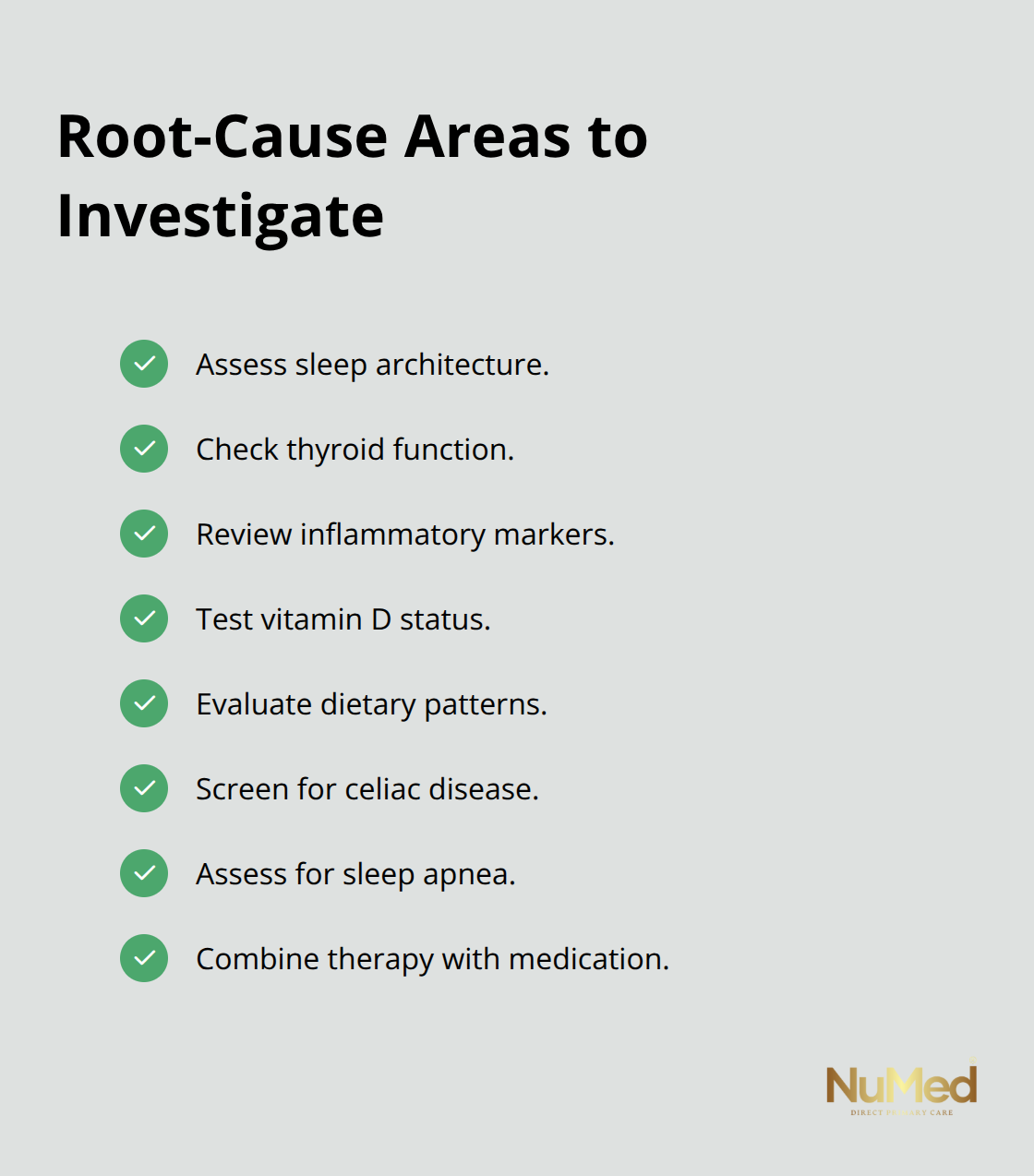
Diagnosis within the medical model follows a systematic process that distinguishes it from other mental health frameworks. A clinician conducts a comprehensive psychiatric evaluation that documents symptom onset, duration, severity, and functional impact across work, relationships, and daily activities. This assessment identifies which diagnostic criteria from the DSM-5 align with the patient’s presentation, establishing a recognized syndrome like major depressive disorder, generalized anxiety disorder, or bipolar II disorder. The evaluation also screens for medical conditions that mimic psychiatric symptoms-thyroid dysfunction, vitamin B12 deficiency, or sleep apnea can produce depression-like presentations- making a thorough medical workup essential before attributing symptoms purely to psychiatric causes.
Evidence-Based Medication Selection
Once diagnosis is established, treatment selection follows evidence-based protocols. SSRIs remain first-line medications for anxiety and depression because clinical trials demonstrate their effectiveness in reducing symptoms. Other classes like serotonin-norepinephrine reuptake inhibitors (SNRIs), atypical antipsychotics, or mood stabilizers address different neurochemical targets depending on the diagnosis. Medication dosing begins conservatively and adjusts based on response and side effects, with clinicians monitoring outcomes through symptom rating scales and patient feedback. Correct dosing and medication selection substantially improve treatment success, while inadequate doses or poor medication matches lead to unnecessary suffering and treatment dropout.
Combining Medication with Evidence-Based Psychotherapy
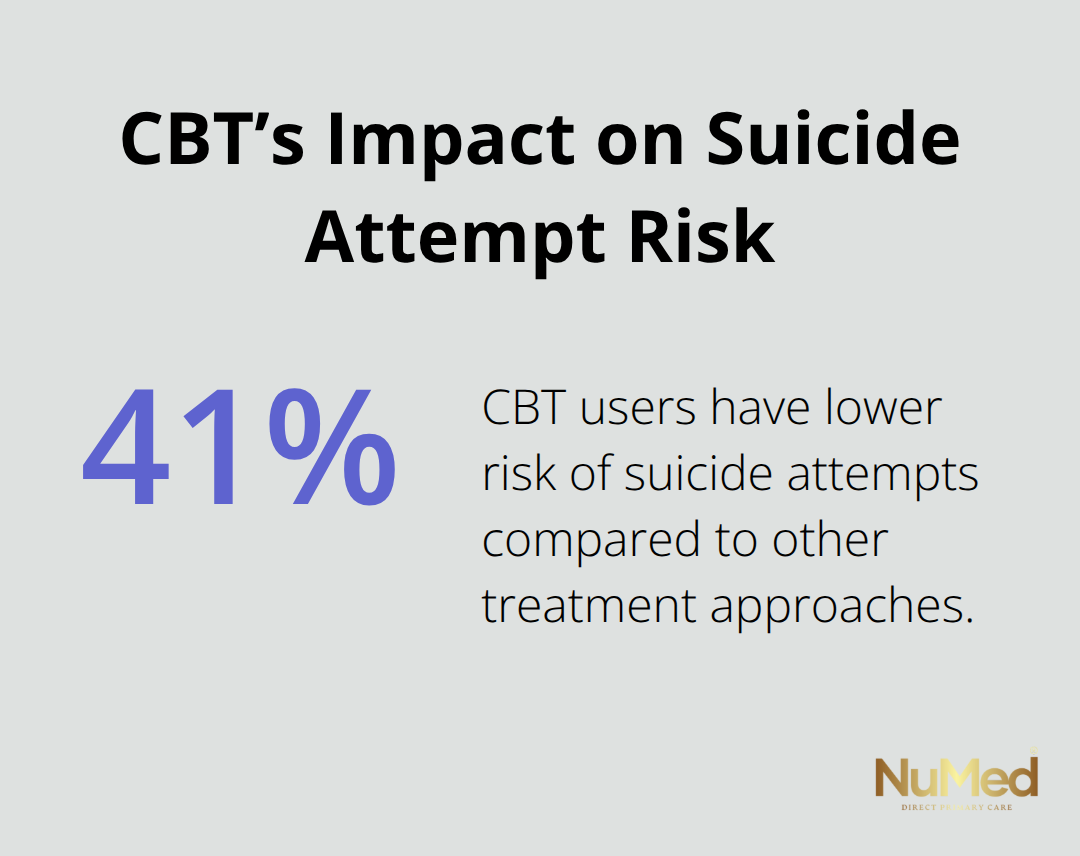
The most effective medical model practice integrates medication management with evidence-based psychotherapy rather than relying on pills alone. Cognitive Behavioral Therapy (CBT) pairs exceptionally well with medication for depression and anxiety, with research showing CBT users have approximately 41% lower risk of suicide attempts compared to other treatment approaches. Dialectical Behavior Therapy (DBT) addresses intense emotions and self-harming behaviors while building mindfulness skills that create measurable brain changes, reducing anxiety and improving stress resilience. Exposure therapy for trauma and phobias, EMDR for processing traumatic memories, and Acceptance and Commitment Therapy (ACT) for chronic conditions all have robust research supporting their use alongside appropriate medications.
Investigating Root Causes Beyond Medication
Integrated care combines medication management with functional medicine investigation, examining sleep quality, nutritional status, hormonal balance, and lifestyle stressors that may drive or perpetuate biological dysfunction. This approach prevents the trap of prescribing higher medication doses when sleep deprivation or nutritional deficiency actually fuels symptoms. Regular follow-up appointments allow clinicians to track medication efficacy objectively, adjust treatment when response plateaus, and catch side effects early. Transparent conversations about medication options, expected timelines for improvement (typically 4-6 weeks before noticeable benefit), and realistic outcome expectations help patients remain engaged in treatment during the critical early phase when discontinuation rates run highest.
Moving Toward Personalized Treatment Plans
The medical model provides a diagnostic framework and pharmacological foundation, yet the most successful outcomes emerge when clinicians move beyond symptom suppression toward sustainable recovery. This requires understanding how biological mechanisms interact with life context, nutrition, sleep patterns, and stress exposure. Patients who receive this comprehensive assessment and treatment approach experience better long-term outcomes than those who receive medication alone. As you evaluate treatment options, the next section explores how limitations of the medical model inform more personalized and holistic approaches to mental health care.
Where the Medical Model Falls Short
The medical model excels at identifying brain chemistry problems and prescribing medications that address them, yet this strength becomes a limitation when clinicians stop investigating why the dysfunction exists in the first place. A patient presenting with depression receives an SSRI prescription within weeks, but nobody asks whether poor sleep quality, untreated sleep apnea, or chronic stress triggered the serotonin depletion. Research from the American Academy of Family Physicians emphasizes that medication alone produces inferior long-term outcomes compared to treatment combining pharmacology with lifestyle intervention and root-cause investigation. The model’s disease-focused framework trains practitioners to match symptoms to diagnoses and select corresponding medications, which works efficiently in acute care but misses the upstream factors perpetuating illness. When a clinician prescribes higher SSRI doses instead of addressing a patient’s nutritional deficiencies, hormonal imbalance, or sleep deprivation, they chase symptoms rather than causes. This approach often leads to polypharmacy, patients accumulating five or six medications to manage side effects and worsening symptoms, when addressing root causes might have prevented escalation entirely.
The Over-Medicalization Problem
The medical model’s reliance on pharmacological solutions creates financial incentives that encourage over-prescription, particularly in primary care settings where mental health screening is common but investigation of root causes is not. Patients with anxiety receive benzodiazepines despite evidence that cognitive behavioral therapy produces equivalent or superior outcomes without addiction risk. Someone diagnosed with mild depression receives antidepressants when sleep optimization, exercise, and social connection might resolve symptoms within weeks. Insurance reimbursement structures reward brief medication management visits over longer assessments exploring lifestyle and environmental factors, making practitioners choose the path of least resistance. The medical model also struggles with medication deprescribing; patients started on psychiatric medications years ago often remain on them indefinitely without reassessment of whether the original problem persists or whether continued medication serves their current needs.
Why Root-Cause Investigation Matters
Sustainable mental health improvement requires combining the medical model’s diagnostic clarity and pharmacological tools with functional medicine investigation, behavioral intervention, and lifestyle modification. A patient with depression benefits from SSRI medication when serotonin dysfunction exists, but also needs assessment of sleep architecture, thyroid function, inflammatory markers, vitamin D status, and dietary patterns. This integrated approach prevents the common scenario where someone takes escalating medication doses while their actual problem, undiagnosed celiac disease, causing neuroinflammation, or untreated sleep apnea, remains invisible. Evidence-based therapy like cognitive behavioral therapy or dialectical behavior therapy addresses thought patterns and emotional regulation skills that medication alone cannot develop.
The most clinically astute practitioners move beyond the medical model’s limitations by treating diagnosis as a starting point rather than the endpoint of assessment. This requires time, curiosity, and willingness to investigate factors outside the neurochemical paradigm-precisely the conditions that direct primary care models create through extended appointments and relationship-focused care.
Building Sustainable Recovery Through Integration
Sustainable recovery emerges when clinicians combine the medical model’s diagnostic framework with functional medicine investigation and behavioral intervention. Extended appointment times allow practitioners to explore sleep quality, nutritional status, hormonal balance, and lifestyle stressors that may drive or perpetuate biological dysfunction. This approach prevents the trap of prescribing higher medication doses when sleep deprivation or nutritional deficiency actually fuels symptoms. Regular follow-up appointments allow clinicians to track medication efficacy objectively, adjust treatment when response plateaus, and catch side effects early. Transparent conversations about medication options, expected timelines for improvement (typically 4-6 weeks before noticeable benefit), and realistic outcome expectations help patients remain engaged in treatment during the critical early phase when discontinuation rates run highest. The most successful outcomes emerge when practitioners investigate what drives the biological dysfunction in the first place rather than stopping at symptom suppression.
Final Thoughts
The medical model mental health framework provides essential diagnostic clarity and evidence-based pharmacological tools that transformed psychiatric treatment over the past seventy years. Medications like SSRIs demonstrably reduce symptoms of anxiety and depression, and structured diagnostic assessment prevents misdiagnosis of treatable medical conditions masquerading as psychiatric illness. Yet this model alone falls short when clinicians stop at symptom suppression rather than investigating root causes.
Individualized treatment planning recognizes that two patients with identical depression diagnoses require entirely different approaches. One person needs medication adjustment plus sleep optimization and nutritional support, while another benefits from cognitive behavioral therapy combined with stress reduction and social connection. A third requires investigation of thyroid dysfunction or inflammatory markers before medication escalation-this personalized assessment takes time and genuine clinical curiosity, which is precisely why extended appointment models produce superior outcomes compared to brief medication management visits.
The future of mental health care integrates the medical model’s diagnostic framework with functional medicine’s root-cause investigation and direct primary care’s relationship-focused approach. We at NuMed DPC recognize that sustainable mental health improvement requires addressing the whole person rather than isolated symptoms. If you’re ready to explore how integrated, personalized mental health care can support your recovery, visit NuMed DPC to learn more about our approach.