Hormonal imbalances affect millions of women, causing fatigue, mood swings, weight gain, and irregular cycles. The good news is that a natural way to balance hormones in women often starts with simple, evidence-based changes to diet, sleep, and stress management.
At NuMed DPC, we believe that understanding your hormones is the first step toward reclaiming your health. This guide walks you through practical strategies to support your body’s natural hormone regulation.
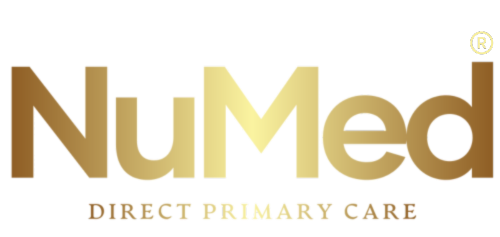
What Your Key Hormones Actually Do
Estrogen, progesterone, testosterone, thyroid hormones, and cortisol form a tightly coordinated network that influences everything from your metabolism to your mood. Estrogen affects bone density, skin elasticity, and cardiovascular health, while progesterone acts as your body’s natural calming hormone, preparing your system for sleep and regulating your menstrual cycle. Testosterone in women drives sex drive, muscle strength, and energy production, even in small concentrations. Thyroid hormones directly control your metabolic rate, meaning imbalances show up as unexplained weight changes or persistent fatigue. Cortisol, your stress hormone, peaks in the morning to wake you and should decline by evening, but chronic stress flattens this rhythm and disrupts sleep, appetite, and immune function.
When these hormones work together properly, you experience stable energy, clear thinking, and regular cycles.
Recognizing Hormonal Imbalance Symptoms
Hormonal imbalances announce themselves through specific, measurable signs that most women recognize but often dismiss as normal aging. Irregular or absent periods, severe PMS, unexplained weight gain around the midsection despite stable eating habits, persistent night sweats, and morning fatigue that coffee cannot fix all point to underlying hormonal dysfunction. Mood swings, brain fog, thinning hair, acne that appears suddenly in adulthood, and a collapsed sex drive are equally reliable indicators. The problem is that these symptoms develop gradually, making it easy to accept them as inevitable. They are not.
How Lifestyle Factors Disrupt Hormonal Function
Lifestyle factors directly influence hormone production, transport, signaling sensitivity, and detoxification. Inadequate sleep shortens your sleep cycles before REM completion, suppressing progesterone and elevating cortisol. Chronic stress keeps cortisol elevated, which then suppresses reproductive hormones. A diet high in refined carbohydrates and low in fiber destabilizes blood sugar, forcing your pancreas to overproduce insulin, which eventually triggers insulin resistance and disrupts the entire hormonal cascade.
The Science Behind Dietary and Lifestyle Changes
The relationship between lifestyle and hormones is not theoretical. A 2021 trial published in Nutrients found that shifting to either a low-calorie Mediterranean pattern or a 30-30-40 macronutrient split (carbs, protein, fat) produced measurable improvements in insulin sensitivity within four weeks. Your food choices directly alter cortisol levels; Mediterranean-style eating lowers fasting cortisol compared to Western diets high in sodium and processed foods, according to research in Nutrients 2024 and Clinical Endocrinology 2020.
Sleep quality matters equally. A cool bedroom at 65 degrees Fahrenheit, consistent sleep timing, and wind-down rituals that exclude screens for one hour before bed support the progesterone surge needed for deep sleep. Exercise timing influences hormone signaling, too. Resistance training two to three times weekly preserves muscle mass and improves insulin sensitivity, while moderate aerobic activity most days supports cortisol rhythm normalization.
Why Stress Management Cannot Be Overlooked
High chronic stress elevates cortisol continuously, which suppresses thyroid hormone activation and impairs leptin signaling, leaving you feeling hungry and fatigued simultaneously. Stress reduction techniques-whether meditation, time in nature, or structured breathing-lower cortisol and restore hormonal rhythm. The evidence shows that women who address stress alongside diet and sleep see faster improvements in cycle regularity and energy levels than those who focus on nutrition alone.
Understanding these connections reveals why hormonal health requires coordinated attention to all these factors rather than isolated interventions. The next section explores which specific foods and nutrients your body needs to support this delicate hormonal balance.
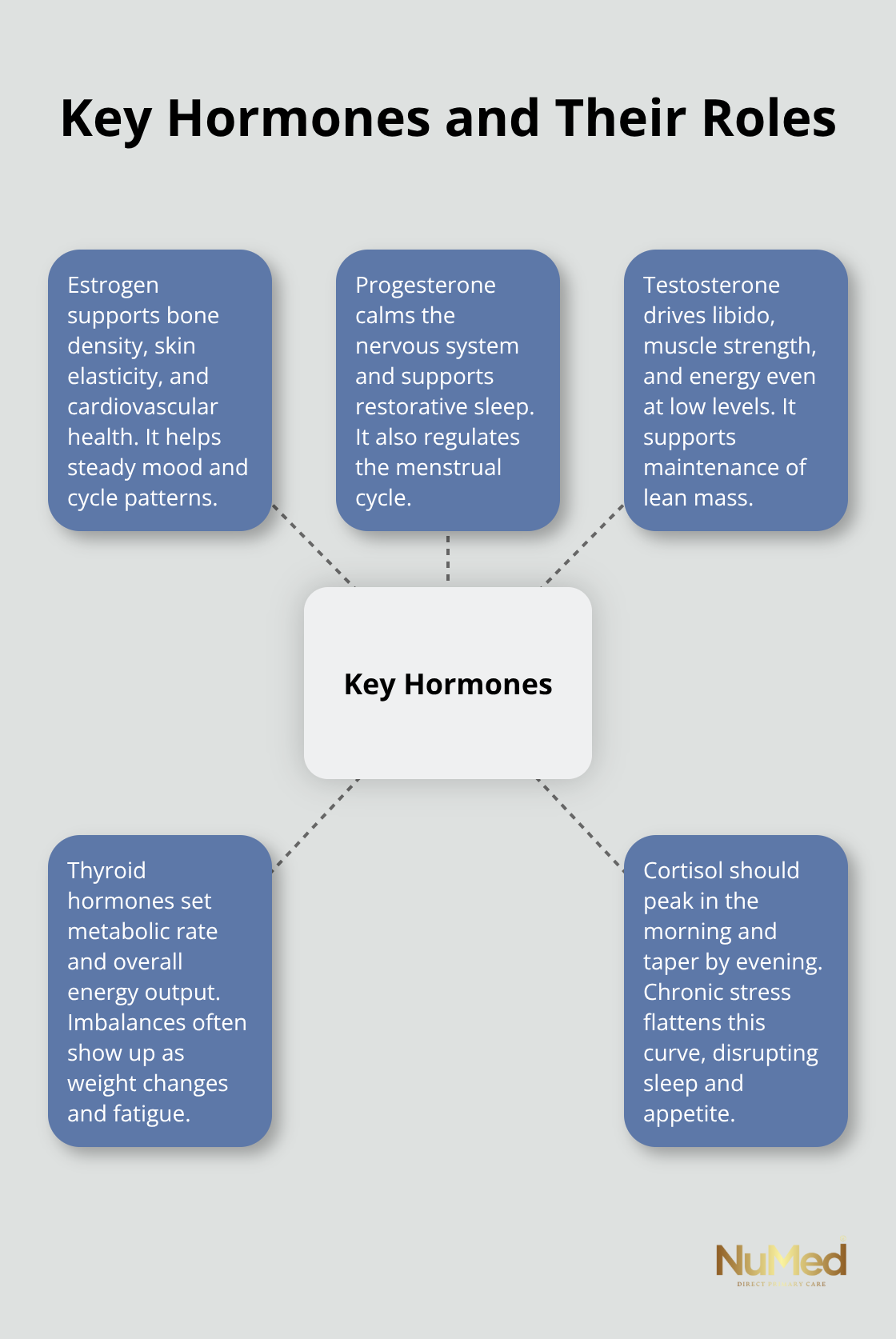
What to Eat for Hormone Balance
Your food choices directly control hormone production and signaling sensitivity within hours of eating. Protein intake matters more than most women realize: targeting 20 to 30 percent of daily calories from protein preserves lean muscle mass, reduces insulin spikes, and lowers androgens in conditions like PCOS. A woman eating 2,000 calories should consume 100 to 150 grams of protein daily, distributed across meals rather than concentrated at dinner. This approach stabilizes blood sugar, keeps you fuller longer, and prevents the afternoon energy crash that triggers cortisol surges and cravings. Practical meals that achieve this balance include eggs with cheese and spinach on whole-grain toast for breakfast, salmon with roasted vegetables and quinoa for lunch, and chicken curry with chickpeas and brown rice for dinner.
The specific pattern matters less than consistency: Mediterranean-style diets and low-glycemic index eating patterns both produce measurable reductions in fasting insulin and improvements in ovulatory function within weeks, according to research published in systematic reviews by Moran and colleagues in 2013 and follow-up trials through 2019.
Blood Sugar Stability Drives Everything Else
Refined carbohydrates without fiber cause insulin to spike and crash repeatedly, eventually triggering insulin resistance that disrupts your entire hormonal network. Instead, prioritize carbohydrates with fiber: legumes, whole grains, vegetables, and fruits, which slow digestion and prevent blood sugar swings. A 2021 trial in Nutrients found that both a Mediterranean pattern and a 30-30-40 macronutrient diet (carbs, protein, fat) improved insulin sensitivity measurably within four weeks, proving that dietary change works fast. Omega-3 fatty acids from fatty fish like salmon and tuna reduce inflammation and improve insulin sensitivity; try two servings weekly. Omega-3 supplementation at therapeutic doses also lowers inflammatory markers like C-reactive protein, directly supporting hormonal signaling. Magnesium-rich foods, including leafy greens, nuts, and whole grains, support insulin action and reduce cortisol; magnesium glycinate supplementation at 200 to 400 milligrams daily helps women with irregular cycles and poor sleep quality.
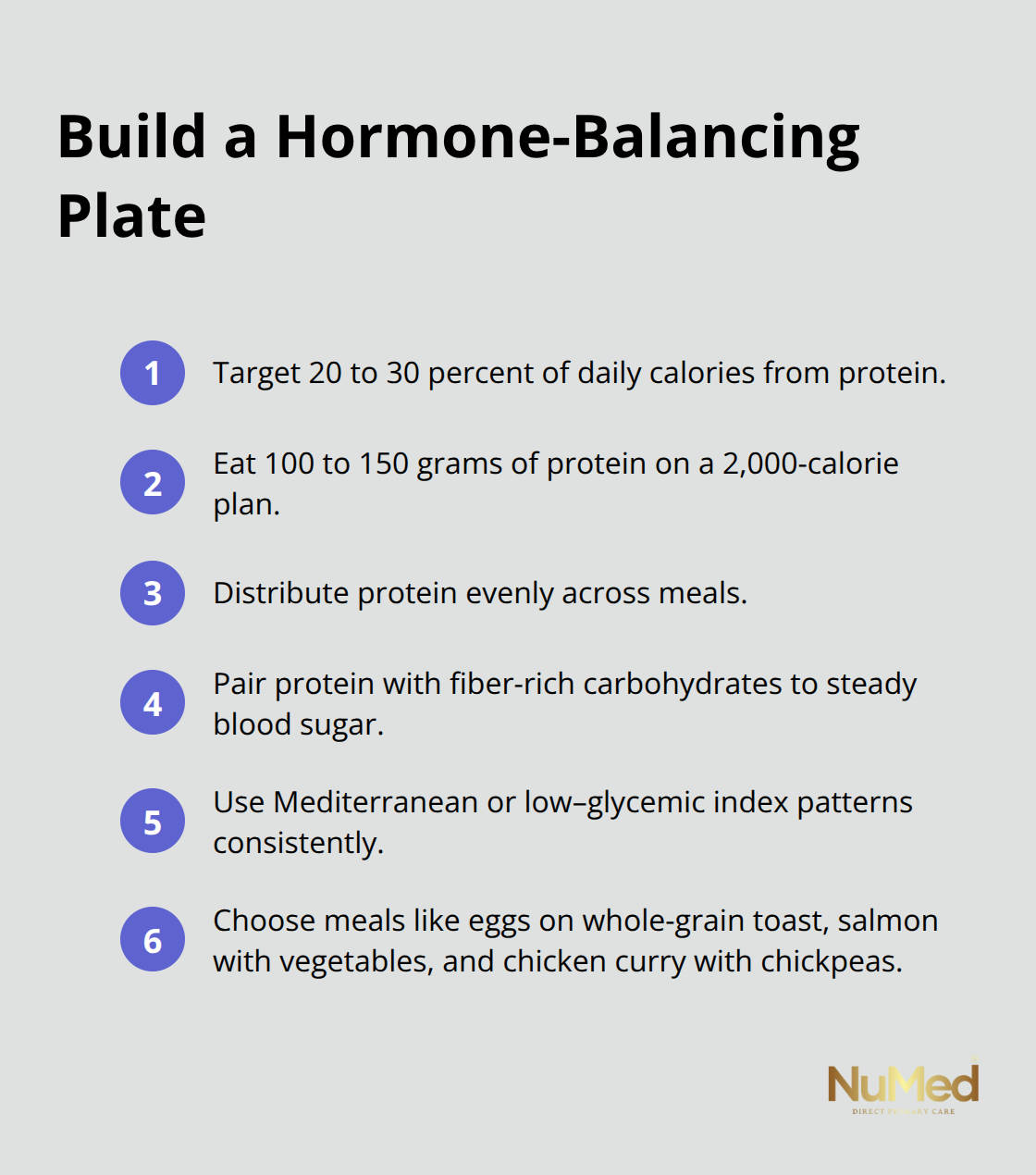
Strategic Supplementation Fills Real Gaps
Vitamin D deficiency affects roughly 40 to 60 percent of women and directly impairs insulin sensitivity and ovulatory function. If testing shows a deficiency, supplementing with 2,000 to 4,000 IU daily improves both metabolic and reproductive outcomes. Myo-inositol at 2 to 4 grams daily improves ovulation rates and insulin resistance, with consistent results across multiple trials.
Cinnamon supplementation at 336 to 1,500 milligrams daily for 6 to 24 weeks lowers fasting glucose and insulin resistance in women with PCOS. Probiotics containing Lactobacillus and Bifidobacterium strains reduce fasting insulin and triglycerides, making them practical additions for women with metabolic dysfunction. N-acetylcysteine at 1,200 to 1,800 milligrams daily for 12 to 24 weeks increases pregnancy rates in PCOS, though this requires medical supervision. Calcium combined with vitamin D improves lipid profiles and insulin resistance when vitamin D status is low. These are not theoretical recommendations: they reflect doses used in published clinical trials showing measurable improvements in hormone markers within weeks to months.
Micronutrient Status Supports Thyroid and Metabolic Health
Adequate selenium, iodine, and iron status directly influences thyroid hormone production and activation. Iodized salt, milk, and seaweed provide iodine; eggs and whole grains supply selenium; legumes and animal proteins deliver iron and zinc. Women with low energy or unexplained weight changes often have suboptimal micronutrient levels that impair thyroid function and insulin signaling. Testing micronutrient status through your healthcare provider reveals whether supplementation will accelerate hormonal recovery. The functional medicine approach recognizes that signaling sensitivity-how effectively your cells respond to hormones-depends on adequate micronutrient cofactors. Correcting deficiencies removes a major barrier to hormonal balance and allows dietary and lifestyle changes to work more effectively.
Your nutritional foundation now supports stable hormones, but sleep quality and exercise timing amplify these gains significantly. The next section explores how to structure your daily movement and rest to optimize hormone production and sensitivity.
Sleep, Movement, and Stress Shape Your Hormonal Reality
Sleep deprivation attacks your hormonal system directly. A bedroom temperature of 65 degrees Fahrenheit triggers the core body temperature drop needed for melatonin release and deep sleep cycles, where progesterone peaks. Warmer rooms or inadequate bedding compress your REM sleep, which suppresses progesterone production and elevates cortisol the following day. Consistent sleep timing matters more than total hours: going to bed at 10 p.m. and waking at 6 a.m. daily stabilizes your circadian rhythm far more effectively than sleeping eight hours at irregular times. One hour before bed, eliminate screens entirely because blue light suppresses melatonin production and delays sleep onset by 30 to 60 minutes on average.
Optimize Sleep Quality With Targeted Strategies
Magnesium glycinate improves sleep quality without the morning grogginess of other forms. Women who prioritize these sleep mechanics see cycle regularity return within one to two menstrual cycles, faster than those relying on diet changes alone. The temperature, timing, and supplement combination work together to restore the hormonal patterns that poor sleep disrupts.
Resistance Training Preserves Muscle and Improves Insulin Sensitivity
Resistance training preserves lean muscle mass, improves insulin sensitivity, and normalizes cortisol rhythm far more effectively than steady cardio alone. Weight-bearing or impact activities like walking, tennis, or jumping rope three to four times weekly strengthen bones and support the metabolic rate that declines with age. Moderate aerobic activity on most days prevents cortisol from remaining elevated throughout the afternoon, which otherwise triggers evening hunger and disrupts sleep.
Avoid the Trap of Chronic High-Intensity Exercise
The critical error most women make is exercising intensely every single day: chronic high-intensity training elevates cortisol continuously, suppressing thyroid hormone activation and worsening fatigue. A sustainable pattern includes two resistance sessions, two moderate aerobic sessions, and one to two lighter movement days like yoga or walking. This structure allows cortisol to recover and hormonal signaling to normalize.
Stress Reduction Lowers Cortisol Within Minutes
Stress reduction techniques lower cortisol directly within minutes. Meditation, breathwork, or time in nature for 15 to 20 minutes daily reduces cortisol more reliably than occasional longer sessions. Women who combine these three elements-sleep optimization, strategic exercise, and daily stress reduction-experience measurable improvements in hormone markers and symptom relief within four to eight weeks (making this combination far more effective than isolated dietary changes).
Final Thoughts
Hormonal imbalances often signal underlying conditions like PCOS, thyroid dysfunction, or insulin resistance that require professional assessment and testing. If you experience irregular cycles lasting more than three months, severe PMS, unexplained weight gain despite consistent eating habits, persistent fatigue unresponsive to sleep improvements, or fertility concerns, professional guidance becomes essential. Testing hormone levels, thyroid function, and metabolic markers reveals whether your symptoms reflect simple lifestyle factors or more complex dysfunction requiring targeted treatment.
The natural way to balance hormones in women works best when guided by someone who knows your complete health picture and can adjust your plan based on real test results rather than assumptions. At NuMed DPC, we specialize in identifying root causes of hormonal dysfunction through comprehensive testing and personalized treatment plans. Our direct primary care model provides the time and attention needed to understand your unique hormonal pattern and design a sustainable recovery strategy.
Start with the foundational changes outlined in this guide, track your symptoms over four to eight weeks, and reach out to a healthcare provider if progress stalls or symptoms worsen. Visit NuMed DPC to learn how personalized primary care can accelerate your hormonal recovery and support lasting health.