Chronic diseases affect over 60% of American adults, yet many patients receive only medication-based treatments that address symptoms rather than root causes.
Lifestyle management for chronic disease offers a proven path to better health outcomes through evidence-based interventions. We at NuMed DPC believe comprehensive care must address nutrition, physical activity, sleep, and stress management together.
This holistic approach can reduce disease progression and improve quality of life significantly.
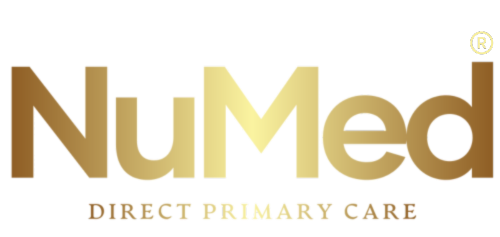
Understanding the Connection Between Lifestyle and Chronic Disease
How Diet Shapes Disease Outcomes
Diet creates the foundation for either disease progression or healing. The American Heart Association found that people who reduce sodium intake to less than 2 grams daily can lower blood pressure by 3.49 mm Hg systolic and 1.96 mm Hg diastolic. Ultra-processed foods increase diabetes risk by 2% per daily serving, while the Mediterranean diet provides consistent cardiovascular protection across populations. Fiber intake of 28-30 grams daily lowers LDL cholesterol and cardiovascular risk significantly. These numbers demonstrate that food functions as medicine when doctors apply it strategically.
Physical Activity Modifies Disease Trajectory
Physical activity acts as a powerful intervention that modifies disease progression at the cellular level. Regular exercise reduces inflammation markers, improves insulin sensitivity, and strengthens cardiovascular function. Patients with diabetes who complete 150 minutes of moderate exercise weekly see A1C reductions of 0.6-0.7%. Resistance training twice weekly prevents muscle loss and improves glucose metabolism in adults over 65. The CDC reports that physical activity reduces the risk of premature death by 30% among adults with chronic conditions (particularly those with heart disease and diabetes).
Sleep Quality Controls Metabolic Function
Poor sleep quality accelerates chronic disease progression through elevated cortisol levels and impaired glucose regulation. Adults who sleep ≤6 hours daily face significantly higher diabetes risk. Sleep deprivation disrupts hormone production and increases insulin resistance within days. Quality sleep allows the body to repair cellular damage and regulate blood sugar levels effectively.
Stress Management Prevents Disease Acceleration
Chronic stress increases inflammatory markers like C-reactive protein, which directly correlates with cardiovascular disease risk. Mindfulness-based stress reduction programs show measurable improvements in blood pressure and pain management within 8 weeks (with some patients seeing results in just 4 weeks). Stress hormones interfere with immune function and accelerate aging at the cellular level. These lifestyle factors work together to create either a disease-promoting or health-supporting environment in your body, which makes comprehensive intervention strategies the next logical step.
Evidence-Based Lifestyle Interventions for Chronic Conditions
Dietary Approaches That Show Clinical Results
The DASH diet stands as the gold standard for hypertension management. Clinical trials demonstrate that this approach reduces systolic blood pressure by 3.2 mm Hg and diastolic by 2.5 mm Hg across diverse patient populations. Patients who follow Mediterranean dietary patterns experience 10-67% reduction in fatal cardiovascular events according to systematic reviews.
Low-carbohydrate approaches increase energy expenditure during weight maintenance phases, while very low-calorie diets produce rapid glucose control improvements in type 2 diabetes within weeks. These dietary interventions work through distinct mechanisms that target inflammation, insulin sensitivity, and metabolic function.
Exercise Protocols Proven to Reduce Symptoms
Structured exercise protocols produce measurable outcomes when patients apply them consistently. Adults with diabetes need exactly 150 minutes of moderate aerobic activity weekly plus two resistance training sessions to achieve 0.6-0.7% A1C reductions. High-intensity interval training shows superior results for cardiovascular fitness improvements compared to steady-state cardio (with sessions as short as 20 minutes producing significant metabolic benefits).
Resistance training twice weekly prevents age-related muscle loss and improves insulin sensitivity in adults over 65. These exercise prescriptions target specific physiological pathways that control blood sugar regulation and cardiovascular function.
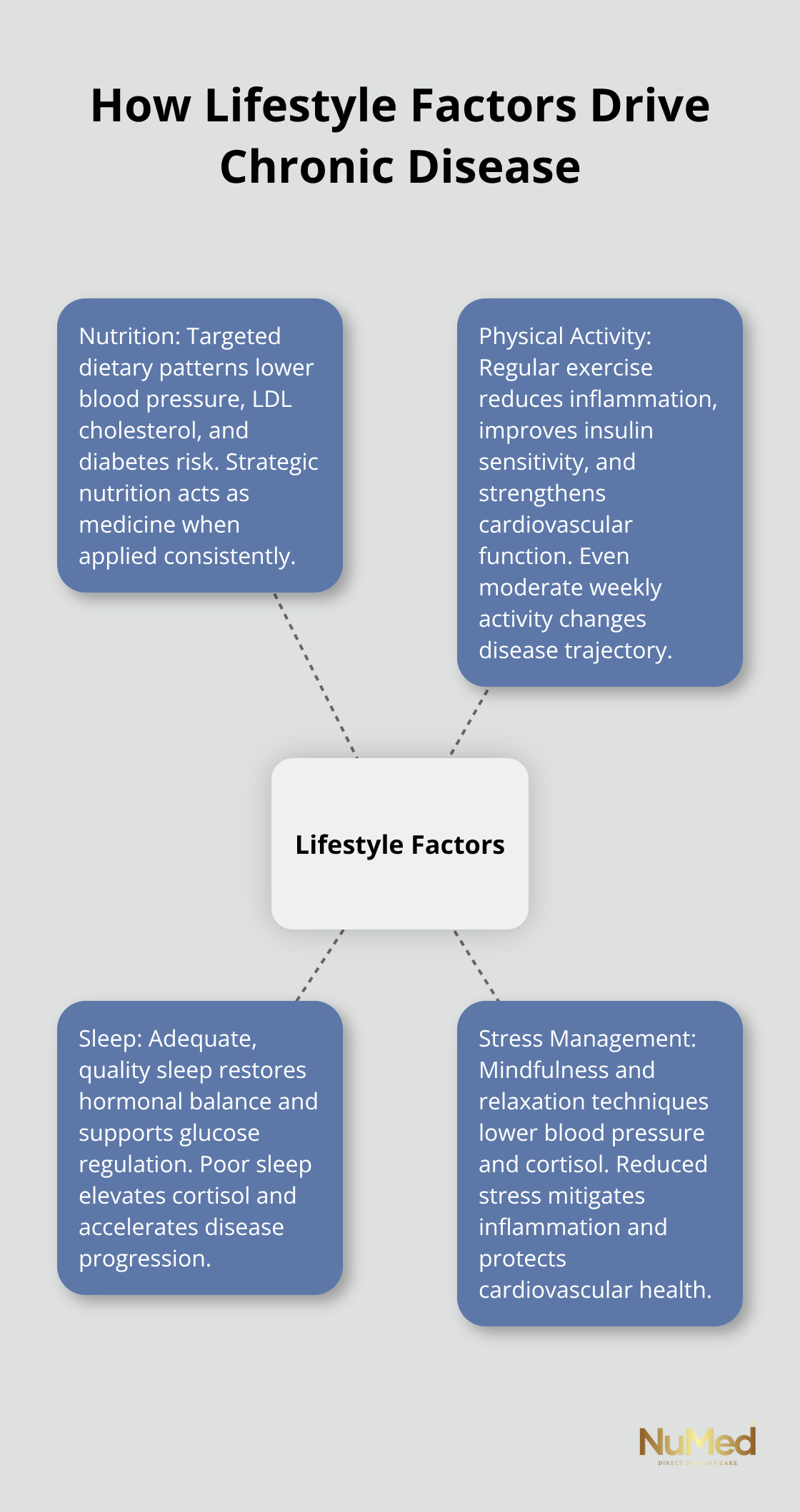
Mindfulness and Behavioral Modification Techniques
Mindfulness-based stress reduction programs demonstrate measurable blood pressure improvements within 8 weeks. Some patients experience benefits in just 4 weeks of consistent practice. Progressive muscle relaxation techniques reduce cortisol levels by 23% when patients practice them consistently for 12 weeks.
Cognitive behavioral therapy approaches show 40-60% improvement rates in chronic pain management and sleep quality scores. These interventions modify stress response patterns and pain perception through neuroplasticity mechanisms (which explains their lasting effects on chronic disease symptoms).
Healthcare providers must monitor progress through regular biomarker testing and adjust protocols based on individual response patterns to maximize these intervention benefits.
Implementing Sustainable Lifestyle Changes
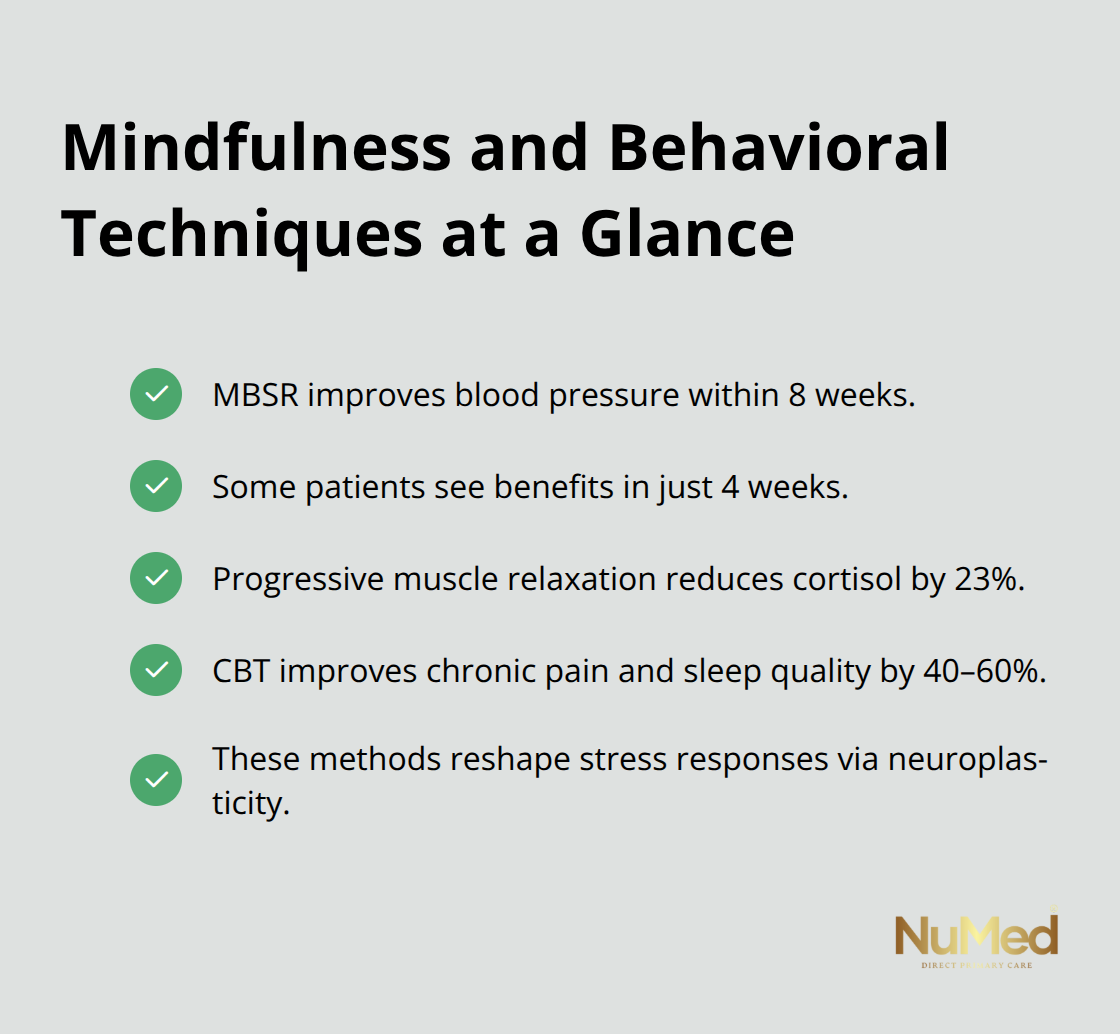
Start Small and Track Specific Biomarkers
Most patients fail because they attempt dramatic changes without measurement systems. The CDC reports that people who track just one health metric daily have 70% higher success rates in lifestyle modification maintenance. Start with morning blood pressure tracking for hypertension patients or fasting glucose for diabetics, rather than multiple variables simultaneously.
Successful habit formation requires 21 days of consistent repetition, according to behavioral psychology research. Focus on single changes like adding 10 minutes of walking after dinner or replacing one processed snack daily. These micro-changes create neurological pathways that support larger modifications later. Patients who master one habit before adding another show 3x better long-term adherence rates.
Build Your Healthcare Support Network
Direct primary care models provide the intensive support structure that chronic disease management requires. Extended appointment times allow comprehensive discussion of lifestyle modifications and barrier identification (which traditional healthcare models often lack due to time constraints).
Your healthcare team should include primary care providers who understand nutrition science, exercise physiologists for movement prescriptions, and behavioral health specialists for stress management. Studies show patients with coordinated care teams achieve 40% better outcomes in diabetes management and 35% greater success in blood pressure control. Regular check-ins every 2-4 weeks during initial habit formation phases prevent backsliding and allow rapid protocol adjustments.
Measure Progress Through Laboratory Values
Subjective improvements mean nothing without objective measurements. A1C levels should drop 0.5-1.0% within 3 months of dietary changes in diabetic patients. Blood pressure improvements appear within 2-4 weeks of sodium reduction and exercise implementation. Inflammatory markers like C-reactive protein decrease within 6-8 weeks of consistent anti-inflammatory dietary patterns.
Schedule laboratory work every 90 days during active lifestyle modification phases. This frequency allows healthcare providers to adjust medication dosages as improvements occur and prevents dangerous interactions between improving health and unchanged prescriptions (a common oversight in traditional care models). Patients who see measurable laboratory improvements maintain motivation 60% longer than those who rely on subjective feelings alone.
Final Thoughts
Lifestyle management for chronic disease produces measurable health improvements that extend far beyond symptom control. Patients who implement comprehensive dietary changes, structured exercise protocols, and stress reduction techniques experience 30-67% reductions in cardiovascular events and significant improvements in diabetes control within months. These interventions modify disease progression at the cellular level through reduced inflammation, improved insulin sensitivity, and enhanced metabolic function.
Personalized care approaches recognize that each patient responds differently to lifestyle interventions. Some diabetics achieve optimal glucose control through low-carbohydrate protocols, while others benefit from Mediterranean dietary patterns. Blood pressure responses vary based on sodium sensitivity and exercise capacity (which requires healthcare providers who understand both the science of lifestyle medicine and the unique circumstances of each patient).
We at NuMed DPC provide the comprehensive support structure that successful lifestyle modification requires. Our direct primary care model allows thorough discussion of lifestyle strategies and regular monitoring of biomarker improvements. Taking action starts with selecting healthcare providers who prioritize prevention and lifestyle intervention alongside appropriate medical treatments.