Menopause affects over 1.3 million women annually in the United States, with 75% experiencing moderate to severe symptoms that disrupt daily life. Natural hormone therapy for menopause offers an alternative approach to managing these challenging symptoms.
We at NuMed DPC understand that choosing the right treatment requires comprehensive information about safety, effectiveness, and personalized care options.
What Makes Natural Hormone Therapy Different
Natural hormone therapy uses bioidentical hormones that match the hormones your body produces naturally. These hormones come from plant sources like soy and yam, then laboratories modify them to match human hormone structures exactly. Traditional synthetic hormone therapy relies on chemically altered hormones from animal sources or laboratory-created compounds that approximate but don’t perfectly match human hormones.
The Women’s Health Initiative study showed that synthetic hormones increased breast cancer risk. Clinical research demonstrates that bioidentical estrogen-only therapy decreased breast cancer incidence compared to synthetic alternatives.
Primary Bioidentical Hormones Used in Treatment
The most effective natural hormones for menopause treatment include estradiol, which addresses hot flashes and bone density concerns. Progesterone balances estrogen and protects the uterine lining from potential complications. Estriol provides gentler symptom relief with lower cancer risk profiles than stronger estrogen forms.
DHEA supports energy levels and cognitive function that often decline after menopause. These hormones work when they bind to the same receptor sites as your natural hormones. This process restores balance without the structural differences that cause many side effects seen with synthetic options.
How Natural Hormones Restore Balance
Natural hormone therapy works when it replaces declining hormone levels with identical molecular structures that your body recognizes and processes normally. The therapy targets specific symptoms through different pathways throughout your system.
Estradiol reduces hot flashes when it regulates temperature control centers in the brain. Progesterone improves sleep quality and mood stability through its calming effects on the nervous system. Studies demonstrate that women who use bioidentical hormone therapy experience 35% to 50% lower risk of coronary heart disease when treatment begins within 10 years of menopause onset.
Research shows significant reduction in overall mortality among menopausal women who start bioidentical therapy early compared to those who use synthetic alternatives or no treatment. These significant health improvements make the choice of therapy type an important decision that affects both immediate symptom relief and long-term health outcomes.
What Health Benefits Can You Expect From Natural Hormone Therapy
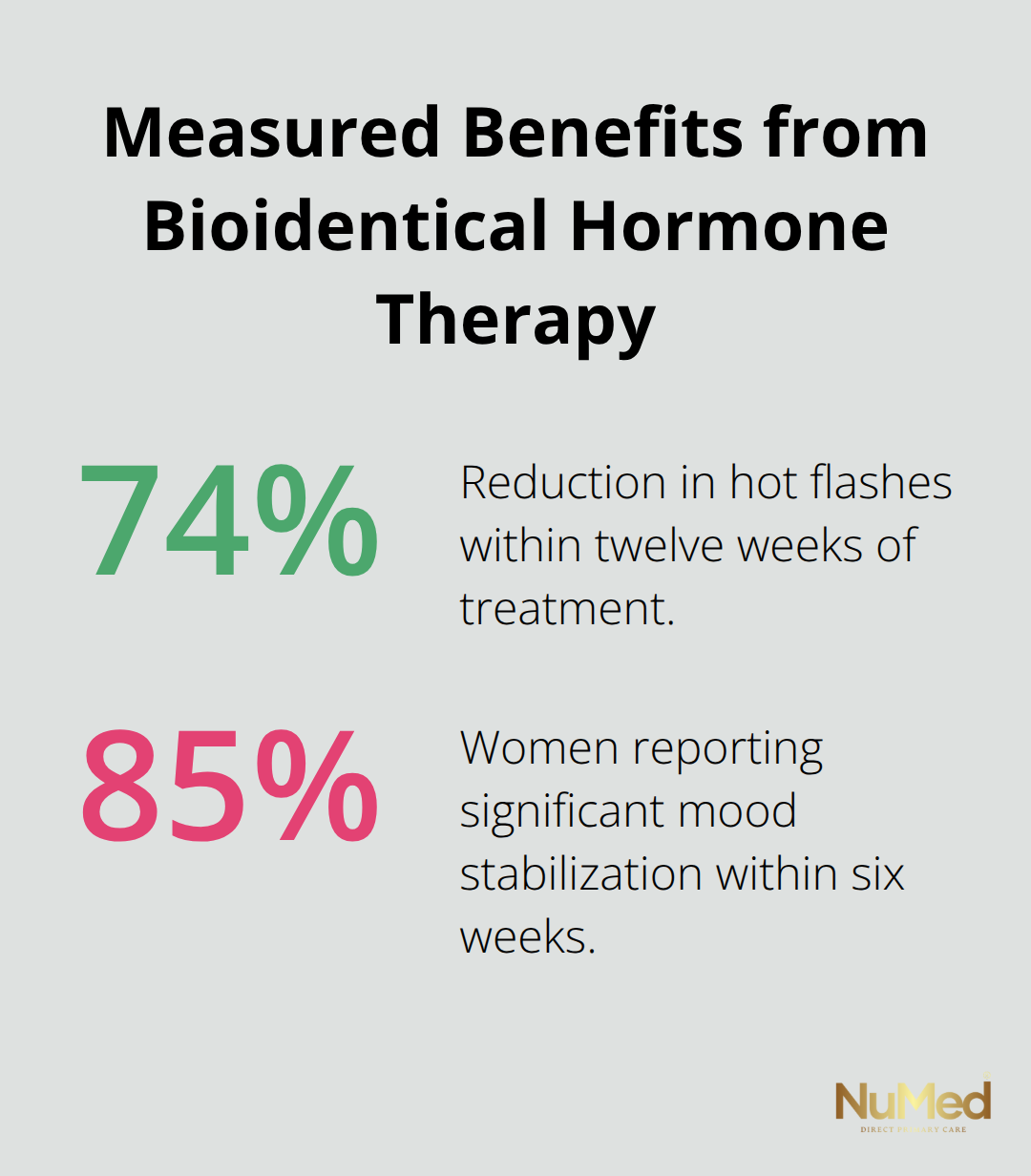
Natural hormone therapy delivers measurable improvements across multiple health areas that extend far beyond basic symptom relief. Women who use bioidentical estradiol report 74% reduction in hot flashes within twelve weeks of treatment according to clinical trial data. Sleep quality improves dramatically when progesterone therapy addresses night sweats and restores natural sleep cycles. The Mayo Clinic reports that 85% of women experience significant mood stabilization within six weeks of starting balanced bioidentical hormone treatment.
Bone Health Protection Through Estradiol Therapy
Estradiol therapy maintains bone mineral density at premenopausal levels when treatment starts within five years of menopause onset. Research published in the Journal of Clinical Endocrinology shows that women who use bioidentical estrogen maintain 98% of their bone density compared to 85% loss in untreated women over five years.
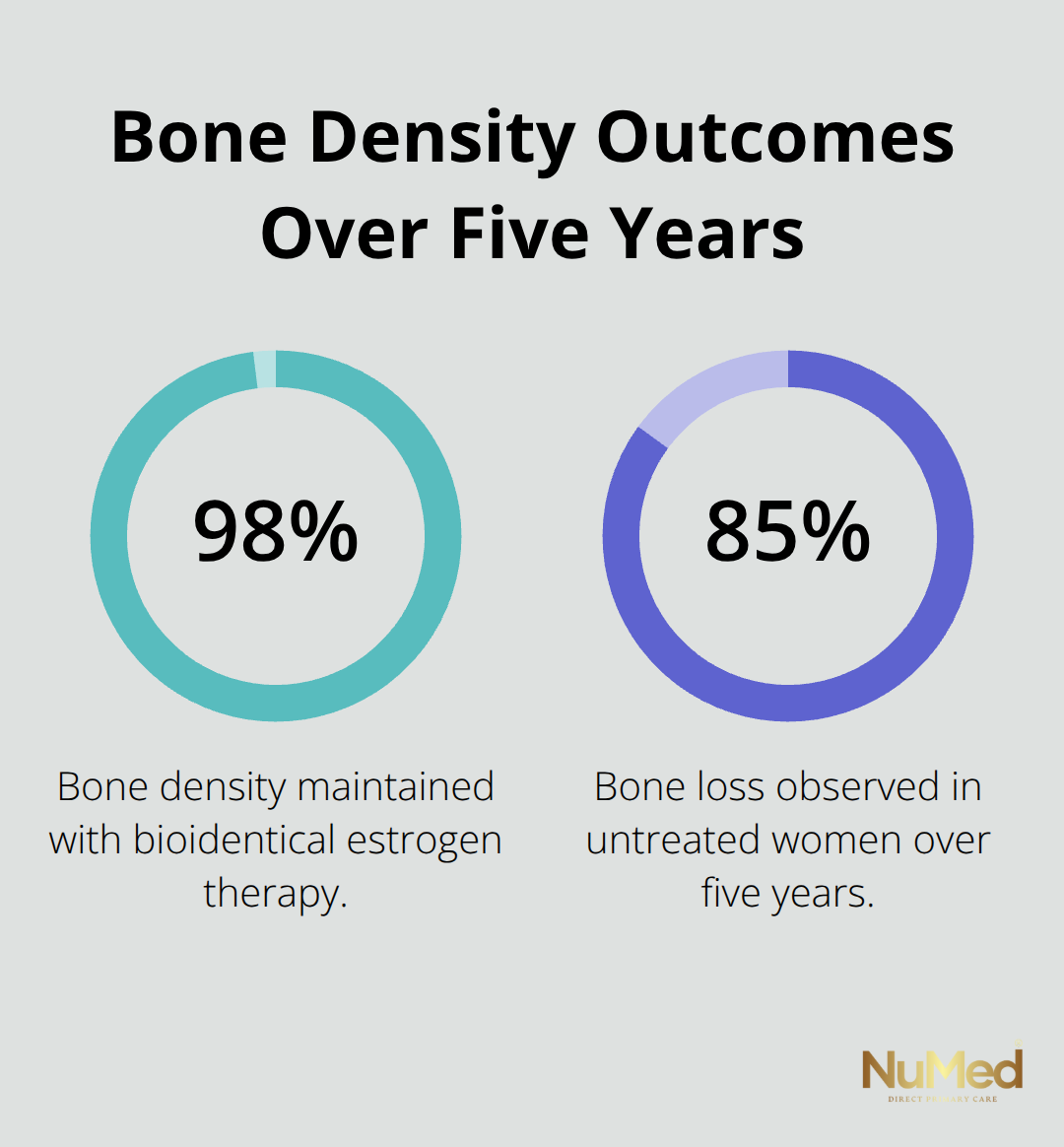
This protection prevents fractures and maintains skeletal strength throughout the postmenopausal years.
Cardiovascular Benefits and Heart Disease Prevention
Cardiovascular protection becomes evident when therapy begins early, though research shows mixed results regarding heart disease prevention in postmenopausal women. Blood pressure regulation improves through estrogen’s positive effects on arterial flexibility and cholesterol metabolism. Women who receive early hormone therapy show improved lipid profiles and reduced arterial stiffness (key markers of cardiovascular health).
Risk Management Through Proper Medical Oversight
Natural hormone therapy carries lower risk profiles than synthetic alternatives, but medical monitoring remains essential for safe treatment. Breast cancer risk varies significantly based on hormone combinations and timing, with estrogen-only therapy that shows protective effects in multiple studies. Women with intact uteruses require progesterone to prevent endometrial hyperplasia, while those who have had hysterectomies can safely use estrogen alone.
Blood clot risk increases minimally with transdermal delivery methods compared to oral administration. Regular mammograms, pelvic exams, and blood work help identify any concerning changes early in treatment. These delivery methods and monitoring protocols form the foundation for safe, effective hormone therapy that your healthcare provider will customize to your specific needs.
Which Delivery Method Works Best for You
Bioidentical hormone pellets offer the most consistent hormone levels with the least daily maintenance. These rice-grain-sized pellets contain crystallized hormones that healthcare providers insert under the skin during a simple office procedure. The pellets release steady hormone amounts for three to six months and eliminate daily dose requirements. These pellets gradually release hormones over three to six months, aiming to maintain more stable levels according to the American College of Obstetricians. Women who use pellet therapy report high satisfaction rates with symptom control and convenience factors.
Topical Applications Provide Flexible Dose Options
Transdermal creams and gels allow precise dose adjustments and reduce liver metabolism that occurs with oral hormones. These preparations absorb through skin directly into bloodstream and avoid first-pass liver processing that can create unwanted metabolites. Transdermal estrogen products may offer advantages over oral dosage forms, including a potentially lower risk of blood clots, and they may be more suitable for certain patients. Application sites rotate between arms, thighs, and abdomen to prevent skin irritation. Most women apply creams twice daily, with hormone levels that peak within two hours and last eight to twelve hours per application.
Injectable Hormone Therapy Options
Injectable bioidentical hormones deliver consistent doses through intramuscular administration every one to two weeks. This method bypasses digestive system processing and provides steady hormone release patterns.
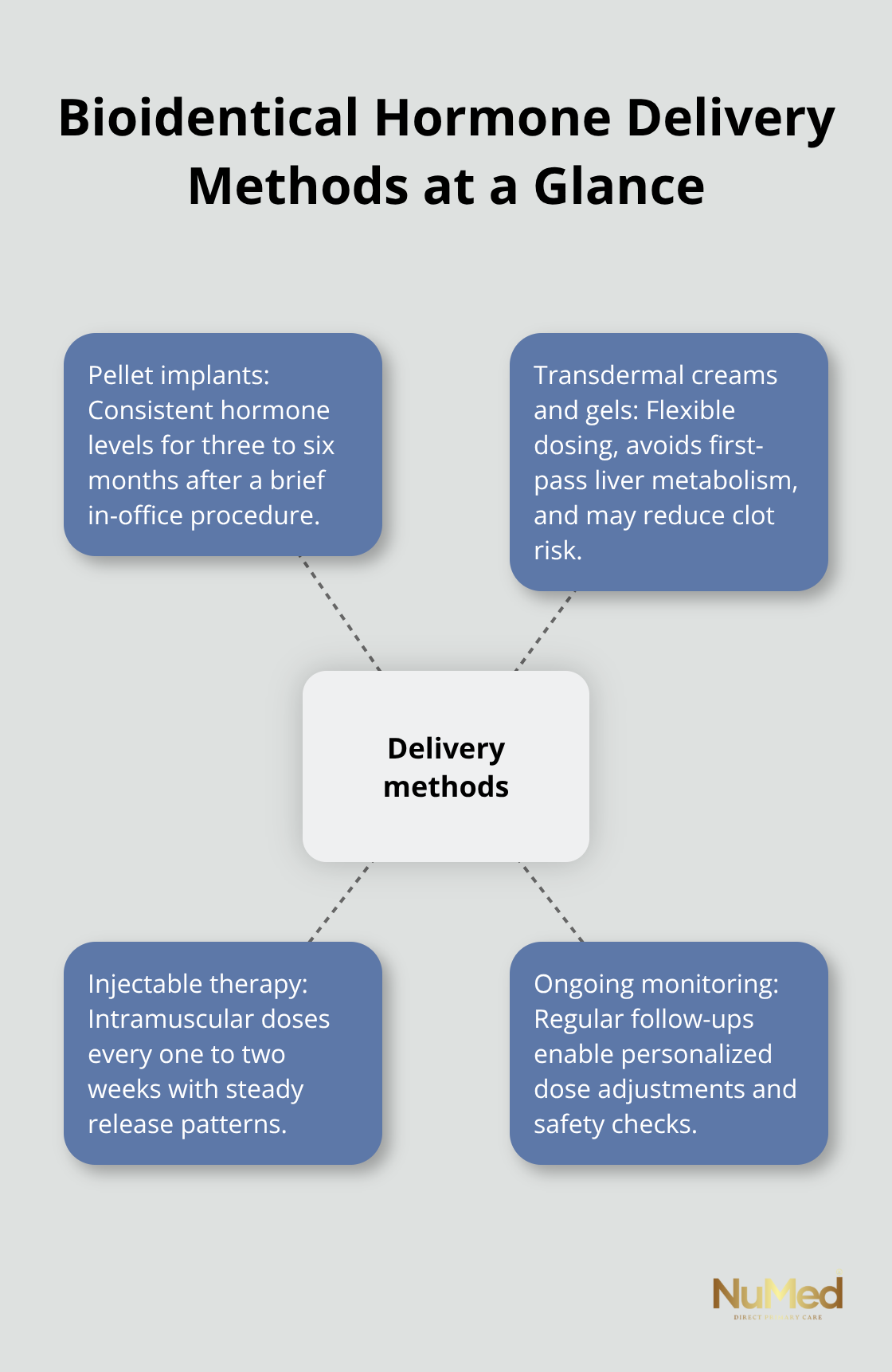
Healthcare providers can adjust injection frequency and dosage based on individual response patterns and symptom relief needs. Many women prefer injections when they want predictable hormone levels without daily applications (though injection schedules require regular clinic visits).
Provider Partnership for Optimal Results
Healthcare providers who specialize in hormone therapy significantly impact treatment success rates. Your provider should order baseline hormone tests, evaluate cardiovascular risk factors, and assess family history before they recommend specific delivery methods. Follow-up appointments every three months during the first year allow dose adjustments based on symptom response and laboratory results. Providers who understand bioidentical hormone therapy can customize combinations and schedules to optimize both safety and effectiveness for your specific health needs.
Final Thoughts
Natural hormone therapy for menopause offers significant advantages over synthetic alternatives, with clinical evidence that shows reduced cancer risks and improved cardiovascular outcomes when treatment begins early. The 74% reduction in hot flashes and maintained bone density at 98% of premenopausal levels demonstrate measurable health benefits that extend beyond symptom relief. Women who choose bioidentical hormones experience fewer side effects and better long-term health outcomes compared to those who use synthetic options.
Personalized medical care forms the foundation of successful treatment. Your healthcare provider should evaluate individual risk factors, order comprehensive hormone tests, and monitor progress through regular follow-ups every three months during the first year. This oversight allows for precise dose adjustments and early detection of any concerning changes (which protects both safety and effectiveness).
Women who consider natural hormone therapy for menopause should schedule consultations with providers who specialize in bioidentical hormone treatment. We at NuMed Direct Primary Care focus on personalized connections between patients and practitioners through comprehensive approaches that include extensive lab services. The decision to begin hormone therapy requires careful consideration of your symptoms, health history, and treatment goals.