Hormonal imbalances affect millions of women, causing fatigue, mood swings, weight gain, and irregular cycles. The good news is that natural remedies for balancing female hormones can make a real difference when you address the root causes.
At NuMed DPC, we focus on functional medicine approaches that go beyond treating symptoms. This guide walks you through proven dietary changes, lifestyle adjustments, and personalized testing to help you reclaim hormonal balance.
Common Hormonal Imbalances in Women
Hormonal imbalances affect millions of women, creating symptoms that range from debilitating to merely annoying. Understanding which imbalance you face helps you target the right natural remedies. Three conditions appear most frequently in women seeking hormone balance.
Estrogen Dominance and Its Symptoms
Estrogen dominance affects women of reproductive age, with this condition occurring when estrogen levels remain elevated relative to progesterone, even if absolute estrogen numbers appear normal on standard blood work. Heavy or prolonged menstrual bleeding, breast tenderness, bloating, mood swings, and weight gain concentrated around the hips and thighs signal this imbalance. Many women experience brain fog and fatigue that worsens before their period.
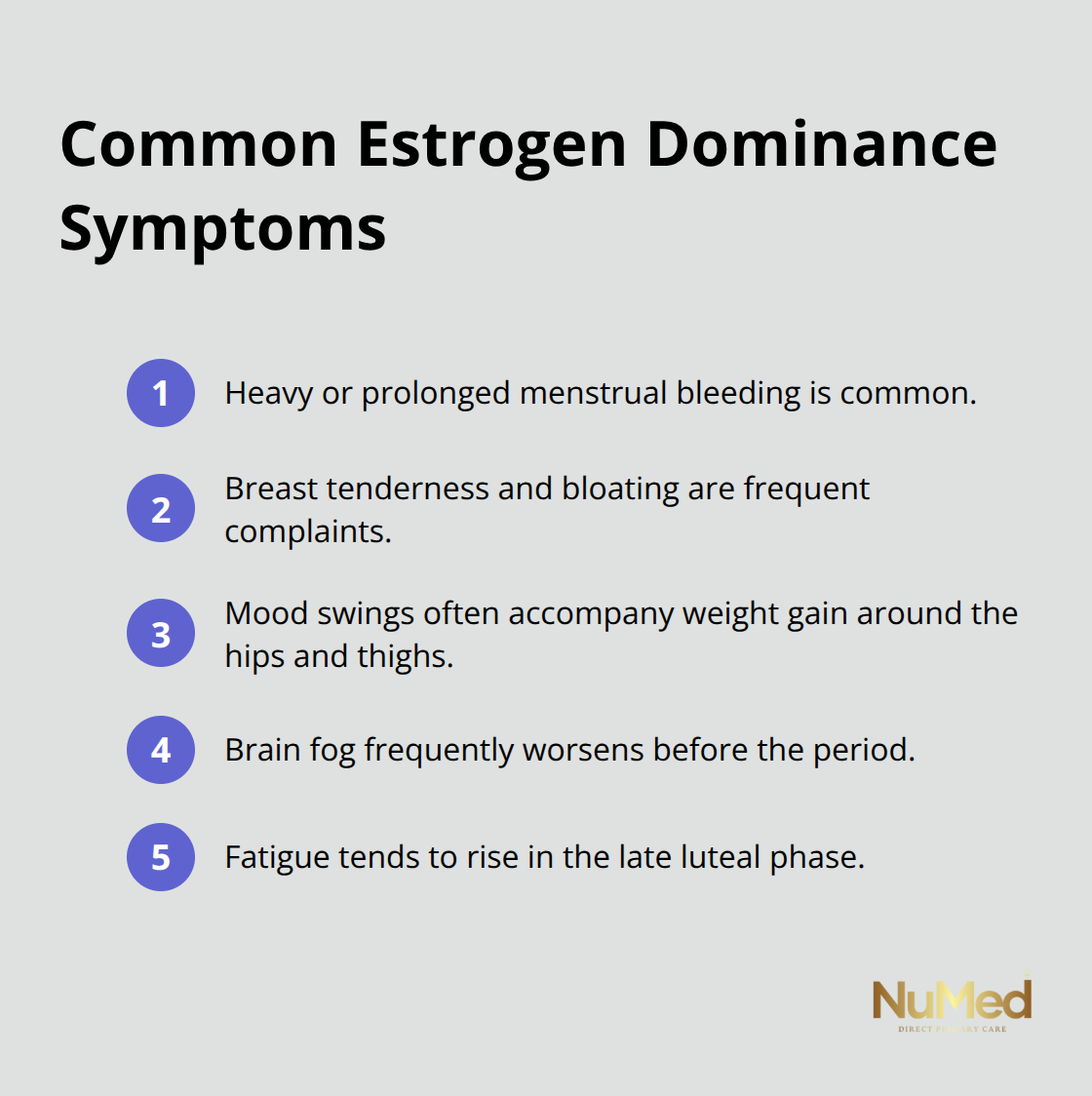
Conventional testing often misses estrogen dominance because it measures only total estrogen levels, not the ratio between estrogen and progesterone. Women with this imbalance typically benefit from reducing exposure to xenoestrogens found in plastics, pesticides on conventional produce, and personal care products. Increasing cruciferous vegetables like broccoli, cauliflower, and Brussels sprouts helps the liver process estrogen more efficiently. These foods contain sulforaphane, a compound that supports phase 2 detoxification.
Progesterone Deficiency Signals
Progesterone deficiency creates a distinct set of problems that differ from estrogen dominance. Low progesterone causes shortened luteal phases, anxiety during the second half of the cycle, insomnia, and difficulty maintaining muscle mass. Women often report feeling wired but tired-a specific combination that points toward progesterone insufficiency.
Magnesium supplementation has evidence supporting its role in progesterone synthesis and mood regulation during the luteal phase. Adequate seed cycling (consuming pumpkin seeds during the follicular phase and sesame seeds during the luteal phase) provides the minerals and lignans needed for hormonal balance. Sleep quality directly impacts progesterone production, and studies show that women sleeping fewer than 7 hours nightly have significantly lower progesterone levels.
Thyroid Dysfunction in Women
Thyroid problems affect women more frequently than men, with thyroid disease affecting a significant portion of women, according to the American Thyroid Association. Hypothyroidism causes fatigue, cold intolerance, hair loss, dry skin, and weight gain despite normal eating habits. Many women receive a normal TSH result and leave their doctor’s office without addressing symptoms because functional medicine practitioners look beyond TSH alone.
Testing free T3, free T4, and thyroid antibodies reveals autoimmune thyroid disease that standard screening misses. Iodine, selenium, and zinc deficiencies impair thyroid function significantly, and women following restrictive diets often lack these minerals. Gut health directly influences thyroid hormone absorption, particularly at the intestinal lining, where T4 converts to active T3. Addressing intestinal permeability through bone broth, zinc carnosine supplements, and eliminating inflammatory foods like refined grains often restores thyroid function without medication adjustment.
Identifying which hormonal imbalance affects you requires proper testing and assessment. The next section explores natural remedies and lifestyle changes that address these imbalances at their source.
How to Eat and Live for Hormone Balance
Protein, Fat, and Vegetables: Your Hormone Foundation
Food choices matter far more than most women realize when balancing hormones. Skip the trendy detox programs and focus instead on what actually rebuilds hormonal health: adequate protein at every meal, healthy fats from sources like salmon and avocados, and vegetables that support liver detoxification. Your liver processes and eliminates excess estrogen, so feeding it properly becomes essential. Try 25 to 30 grams of protein at breakfast alone, as this stabilizes blood sugar and prevents the insulin spikes that worsen hormonal imbalances. Women who eat sufficient protein report fewer mood swings and more stable energy throughout their cycles.
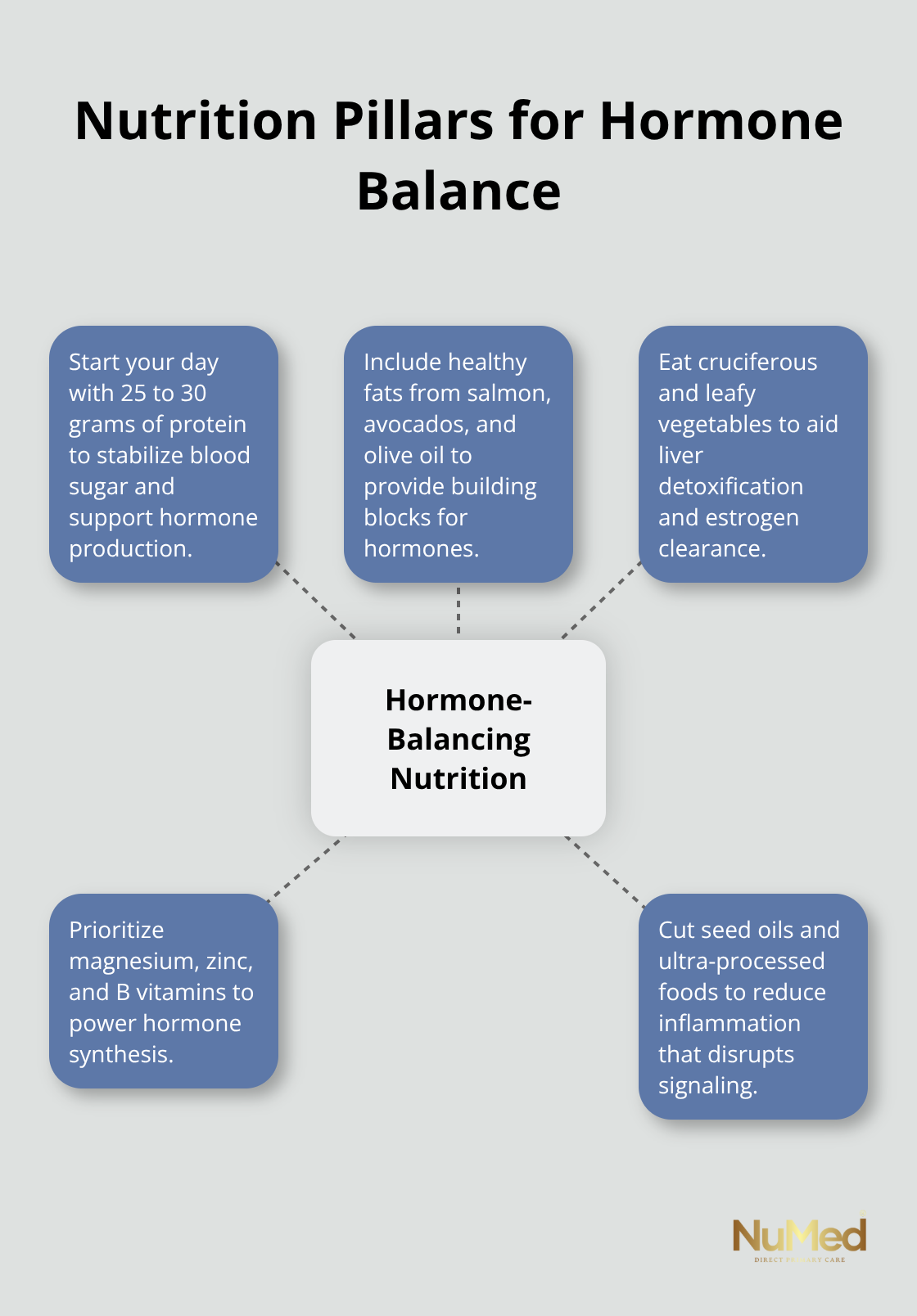
Include leafy greens, cruciferous vegetables, and colorful produce daily to provide the micronutrients your body needs for hormone production. Magnesium, zinc, and B vitamins become non-negotiable, not optional supplements. Reduce seed oils and processed foods aggressively, as these promote inflammation that disrupts hormonal signaling. The Standard American Diet creates estrogen dominance through processed foods and xenoestrogens, so real food becomes your most powerful medicine.
Sleep: The Non-Negotiable Priority
Sleep and stress management are not secondary concerns but primary drivers of hormonal health. Prioritize sleep before considering any supplement. Implement a non-negotiable wind-down routine starting 90 minutes before bed: dim lights, stop screen exposure, and reduce mental stimulation.
Stress Resilience and Recovery
Cortisol dysregulation from chronic stress suppresses progesterone production and worsens every hormonal imbalance discussed earlier. Cold exposure from brief showers or ice baths improves stress resilience, though start conservatively with 30-second exposures. This practice strengthens your nervous system’s ability to handle daily stressors without tanking hormone production.
Exercise That Matches Your Cycle
Movement matters tremendously, but the type depends on your cycle phase. During the follicular phase, higher-intensity exercise like running or strength training works well because estrogen rises and supports performance. During the luteal phase, switch to lower-intensity movement like walking, yoga, or swimming because progesterone rises and requires gentler exertion. This cyclical approach prevents overtraining, which tanks progesterone and worsens PMS symptoms.
These dietary and lifestyle foundations create the conditions for hormonal healing. However, identifying which specific imbalances affect you requires proper assessment and testing-something that functional medicine practitioners address through comprehensive evaluation rather than standard lab work alone.
The Role of Functional Medicine in Hormone Health
Standard lab testing uses population-wide reference ranges that fail to identify hormonal dysfunction in individual women. Your TSH might fall within normal limits while your free T3 remains low, leaving you fatigued and unable to lose weight. Your total estrogen appears acceptable, yet your estrogen-to-progesterone ratio creates dominance symptoms. Functional medicine practitioners measure what conventional medicine ignores: the relationships between hormones, not just absolute numbers.
Hormonal health depends on these ratios and individual baselines rather than generic reference ranges. A woman feeling exhausted and anxious needs different testing than someone with heavy bleeding, yet conventional medicine often orders identical panels for both. Functional assessment starts with comprehensive hormone panels that include free T3, free T4, thyroid antibodies, progesterone, estradiol, and cortisol patterns across the day.
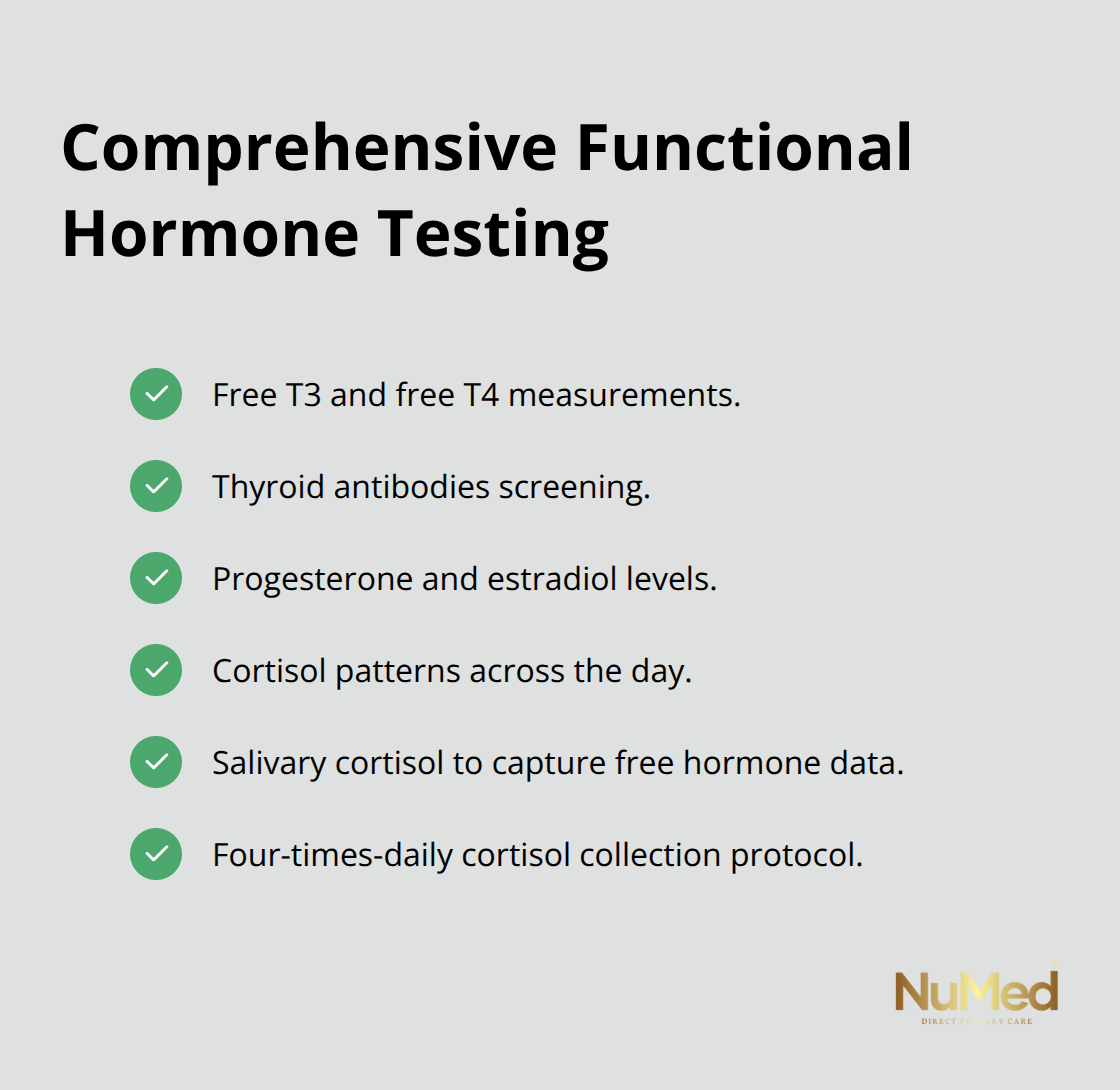
Testing cortisol four times daily reveals whether your body maintains healthy stress response patterns or crashes by afternoon. Saliva testing captures free cortisol that blood tests miss, providing actionable data about your actual hormonal state rather than snapshots that hide dysfunction.
Root Cause Investigation Changes Everything
Finding the cause of hormonal imbalance matters infinitely more than naming the symptom. A woman with low progesterone might have insufficient luteinizing hormone from pituitary dysfunction, poor ovulation from insulin resistance, or inadequate cholesterol intake needed for progesterone synthesis. Each cause requires a completely different treatment.
Functional practitioners spend time investigating your health timeline, identifying when symptoms started and what preceded them. Did your hormone problems begin after a viral infection, prolonged stress, antibiotic use that damaged gut bacteria, or dietary restriction? The answer determines treatment direction. Standard medicine treats the symptom with medication, while functional medicine investigates why your body stopped producing adequate hormones.
Gut dysbiosis directly impairs estrogen metabolism because your microbiome produces beta-glucuronidase, an enzyme essential for estrogen elimination. Women with imbalanced gut bacteria recirculate estrogen instead of eliminating it, creating dominance that supplements alone cannot fix. Assessing your complete health picture through detailed history, comprehensive testing, and targeted investigation reveals whether your thyroid problem stems from autoimmunity, iodine deficiency, or poor conversion of T4 to active T3. Each requires a different intervention.
Personalized Protocols Beat One-Size-Fits-All Solutions
Once root causes emerge from proper assessment, treatment becomes highly specific rather than generic. A woman with estrogen dominance from poor liver detoxification needs cruciferous vegetables and liver-supporting supplements like milk thistle and NAC, while someone with dominance from gut dysbiosis needs probiotic restoration and specific dietary modifications. The same symptom requires entirely different approaches depending on the causation.
Personalized protocols account for your existing nutrient deficiencies, digestive capacity, medication interactions, and health goals. Someone taking levothyroxine needs different timing and support than someone managing hypothyroidism through dietary modification alone. Your treatment plan adapts as testing reveals progress, shifting strategies when initial approaches plateau (this responsiveness distinguishes functional medicine from both conventional medicine’s static prescriptions and the supplement industry’s generic recommendations).
Ongoing reassessment through repeat testing every 6 to 12 weeks allows your protocol to evolve as your hormones rebalance. This personalized, investigative approach requires more time and attention than conventional medicine typically provides, but the results justify the investment through actual hormonal restoration rather than symptom suppression.
Final Thoughts
Hormonal balance requires investigation into root causes rather than chasing symptoms with generic solutions. Estrogen dominance from poor liver detoxification needs completely different support than dominance stemming from gut dysbiosis, and this distinction separates women who struggle indefinitely from those who actually recover. Your foundation starts with adequate protein at every meal, daily vegetables that support detoxification, consistent sleep, and movement that matches your cycle phase-these lifestyle changes alone resolve hormonal problems for some women.
Knowing when to seek professional guidance matters tremendously if you’ve implemented dietary changes and lifestyle modifications for three months without improvement. Standard lab work often misses hormonal dysfunction because it uses population-wide reference ranges instead of measuring the ratios and patterns that reveal individual imbalance. Functional practitioners investigate your complete health timeline, order comprehensive hormone testing, and create personalized protocols that evolve as your body responds to natural remedies for balancing female hormones.
Taking control of your hormonal health means moving beyond generic advice toward investigation and personalization. NuMed DPC focuses on preventing illness by addressing root causes through functional medicine and health coaching tailored to your unique needs, providing the time and attention required for genuine hormonal restoration rather than symptom suppression.