One-size-fits-all medicine is becoming obsolete. What is personalized healthcare, and why should it matter to you?
At NuMed DPC, we believe tailored treatment based on your unique genetic makeup, medical history, and lifestyle produces better outcomes than standard protocols. This guide walks you through how personalized medicine works and why it’s reshaping patient care.
How Personalized Healthcare Beats the Traditional Model
Traditional medicine treats patients according to established protocols that apply broadly across populations. A doctor diagnoses high blood pressure and prescribes the same medication class to most patients, regardless of whether their condition stems from sodium sensitivity, stress, or genetic factors. Personalized healthcare rejects this approach entirely. Instead of following a standard playbook, personalized medicine identifies what makes your biology unique-your genetic makeup, biomarker profile, and metabolic patterns-then builds treatment around those specifics.
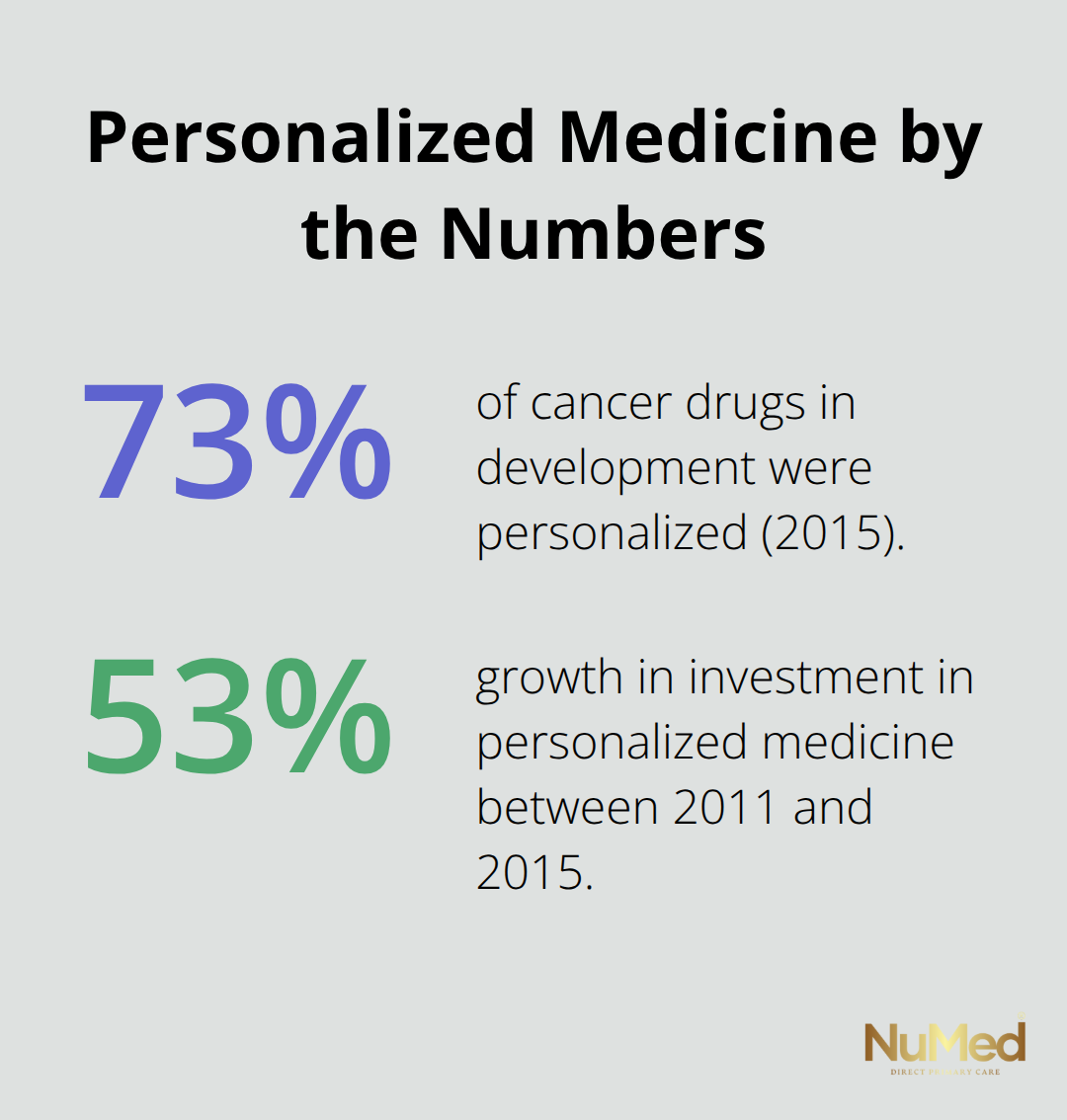
The difference is not subtle. When oncologists use biomarker testing to match cancer patients with targeted drugs, response rates improve dramatically compared to chemotherapy administered without genetic insight. As of 2015, 73 percent of drugs in development for cancer were personalized, signaling that precision matching has become the industry standard in oncology. This shift reflects a hard truth: one-size-fits-all medicine wastes time, money, and patient health on treatments that don’t work for individual biology.
Your Genetic Code Determines What Works
Your DNA contains instructions that affect how you metabolize medications, respond to lifestyle changes, and develop disease. Traditional practitioners rarely access this information. Personalized healthcare practitioners order genetic testing and biomarker panels to reveal these patterns. Someone with genetic variations affecting how they process certain blood pressure medications might respond better to a different class entirely. Another patient’s chronic fatigue might trace to a specific metabolic dysfunction that standard lab work misses.
The global biomarker market reached 51.5 billion dollars in 2024, reflecting massive investment in diagnostic tools that identify these individual differences. When you know your genetic and molecular profile, treatment becomes targeted rather than experimental. Practitioners investigate what your specific biology requires rather than defaulting to conventional wisdom.
Prevention Replaces Reactive Treatment
Traditional medicine waits for disease to appear, then responds with medication or surgery. Personalized healthcare operates differently. Armed with your biomarkers, family history, and genetic risk factors, practitioners identify disease risk before symptoms emerge. Someone carrying genetic markers for early-onset heart disease can begin targeted interventions decades before a heart attack occurs. Another person with metabolic markers suggesting diabetes risk can modify diet and lifestyle with precision, knowing exactly which interventions address their specific dysfunction.
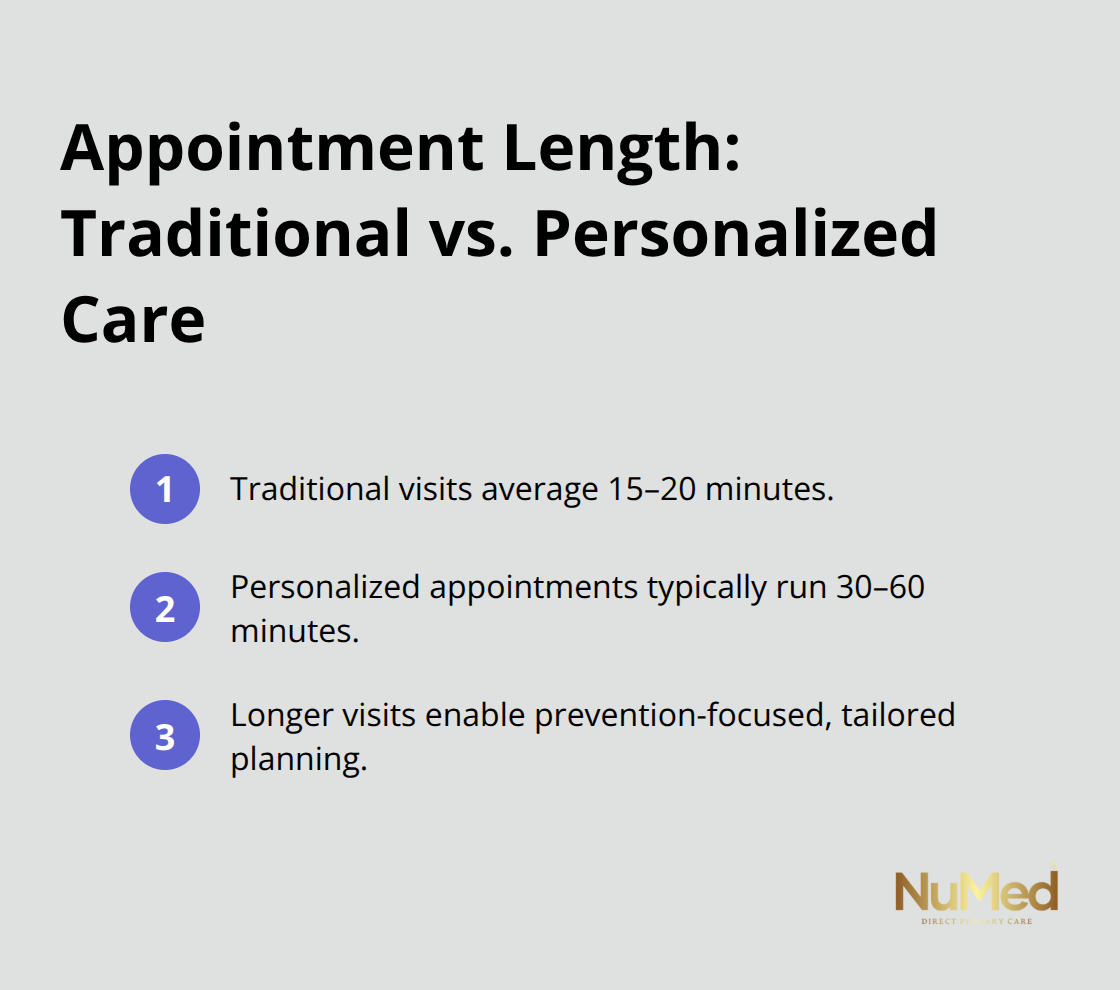
This preventive stance reduces hospitalizations and expensive interventions over time. Longer appointment times in personalized care models enable practitioners to discuss these findings thoroughly and build realistic treatment plans tailored to your life. Traditional visits average 15 to 20 minutes; personalized healthcare appointments typically run 30 to 60 minutes, allowing time for the detailed conversation that prevention requires.
How Technology Enables Tailored Treatment
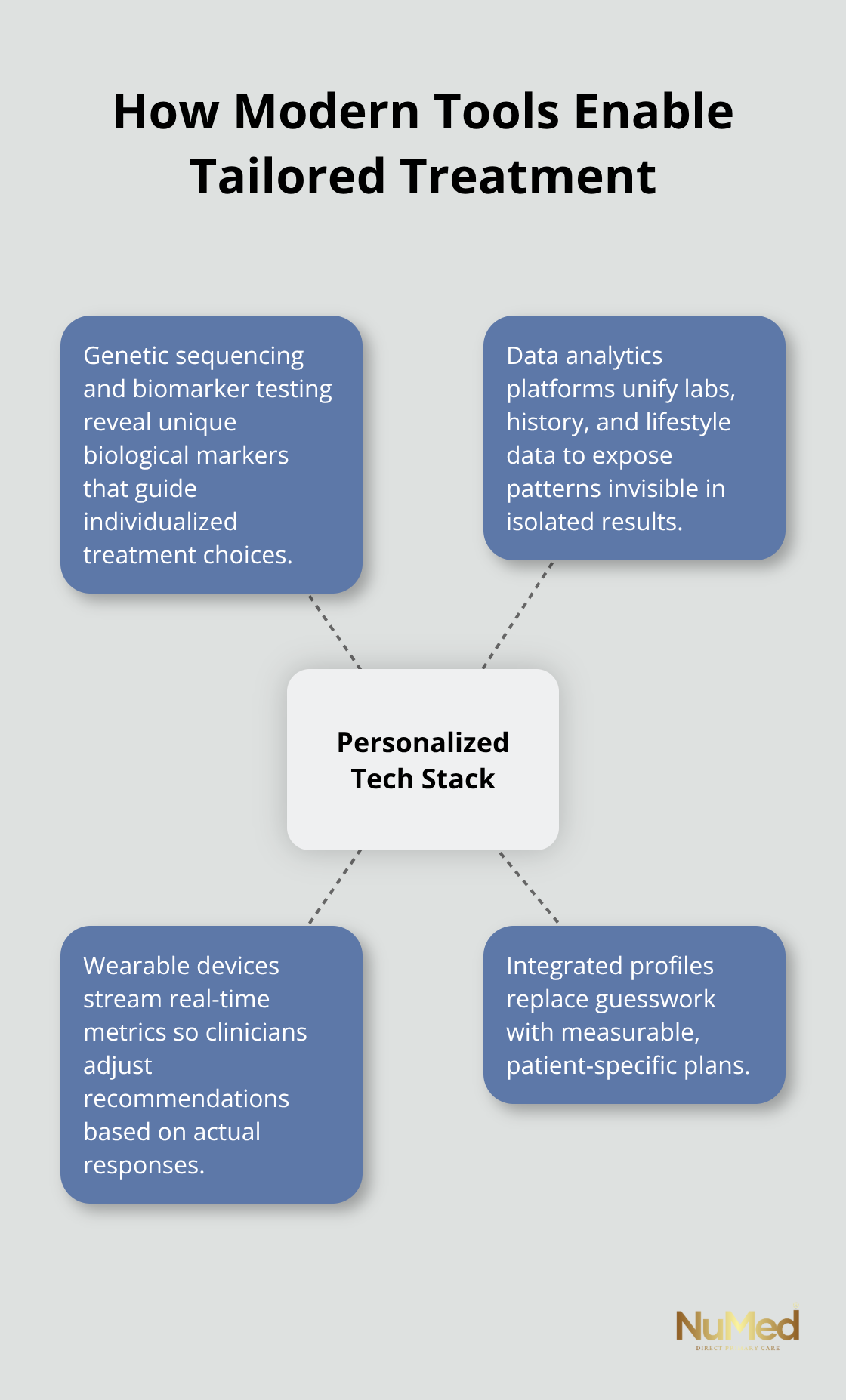
Advanced diagnostic tools now make personalized medicine accessible beyond academic medical centers. Genetic sequencing costs have fallen dramatically, and biomarker testing has become routine in many practices. Data analytics platforms integrate your test results, medical history, and lifestyle information into a comprehensive profile that guides treatment decisions. Wearable devices (fitness trackers, continuous glucose monitors, heart rate monitors) feed real-time data into these systems, allowing practitioners to adjust recommendations based on how your body actually responds.
This technological foundation transforms the patient-practitioner relationship. Instead of guessing whether a treatment works, you and your doctor track measurable outcomes and modify the plan accordingly. The shift from reactive to preventive care transforms not just how often you see a doctor, but why you see them at all-moving you toward understanding your unique health trajectory and the specific interventions that matter most for your biology.
How Modern Tools Transform Treatment Decisions
Genetic testing moves from labs to clinical practice
Genetic sequencing and biomarker testing have moved from research laboratories into clinical practice, making personalized diagnosis accessible to ordinary patients. Today, comprehensive genetic panels cost between 200 and 800 dollars and return results within days. This speed matters because treatment decisions cannot wait. When a patient presents with unexplained fatigue or resistant hypertension, rapid biomarker testing identifies metabolic dysfunction, hormonal imbalances, or genetic variations that standard bloodwork misses entirely.
Data Analytics Reveal Hidden Patterns
Data analytics platforms consolidate genetic information, lab results, medication history, and lifestyle factors into unified patient profiles that reveal patterns invisible in isolated test results. A patient might show normal cholesterol on standard lipid panels but carry genetic markers indicating cardiovascular risk, or metabolic data suggesting insulin resistance before blood sugar levels spike. These platforms flag these connections automatically, prompting practitioners to intervene early with targeted nutrition, exercise protocols, or medication adjustments calibrated to individual biology. Forward-thinking clinics integrate these results directly into treatment planning, matching interventions to measurable biological markers rather than guessing based on symptoms alone.
Wearable Technology Enables Real-Time Monitoring
Wearable technology has transformed how practitioners monitor treatment effectiveness between office visits. Continuous glucose monitors, advanced fitness trackers, and smartwatch-integrated heart rate variability sensors generate thousands of data points monthly, revealing how your body responds to specific interventions in real time. Someone starting a new blood pressure medication no longer waits three months for the next appointment to assess effectiveness; practitioners review weekly data trends and adjust dosing or switch medications within days if needed.
Sleep trackers correlate rest quality with mood, inflammation markers, and medication timing, exposing relationships that patients never notice alone. This continuous feedback loop eliminates the traditional healthcare delay where problems fester undetected between annual visits. Practitioners armed with wearable data catch medication side effects, dietary triggers, and lifestyle factors sabotaging treatment outcomes before they cause harm. The shift from periodic snapshots to continuous monitoring represents a fundamental change in how treatment gets refined, moving from reactive adjustments to proactive optimization based on your actual physiological responses rather than population-level assumptions.
Integration Creates Accountability and Precision
When genetic data, analytics platforms, and wearable monitoring work together, treatment becomes measurable and accountable. Your practitioner no longer relies on your memory of whether you took medications consistently or followed dietary recommendations. The data speaks for itself. Wearable devices document sleep patterns, activity levels, and physiological stress markers. Lab work tracks how your body metabolizes treatments. Genetic profiles predict which interventions will work before you waste time on ineffective options. This integration transforms healthcare from a guessing game into a science tailored specifically to your biology, empowering you to control your health journey.
The next section explores how these tools translate into real-world health improvements, showing what happens when practitioners apply personalized data to actual patient care.
Where Personalized Healthcare Delivers Real Results
Personalized healthcare transforms abstract medical data into concrete health improvements that patients notice and measure. When practitioners match treatments to your genetic makeup and biomarker profile, response rates climb dramatically compared to standard protocols. Cancer patients treated with drugs selected through genetic testing show significantly higher remission rates than those receiving chemotherapy without biomarker guidance, a principle now standard across oncology. The same precision applies to chronic disease management. A patient with resistant hypertension caused by specific genetic variations responds within weeks to a targeted medication class, whereas years of trial-and-error dosing might have failed under traditional approaches.
Medication Side Effects Disappear When Treatment Matches Biology
Adverse drug reactions represent one of the leading causes of preventable death in hospitals. Many of these deaths stem from prescribing medications that a patient’s genetics cannot tolerate. Genetic testing identifies cytochrome P450 variations that determine how rapidly your liver metabolizes specific drugs. Someone carrying slow-metabolizer variants accumulates dangerous drug levels on standard doses, while fast metabolizers achieve no therapeutic benefit from the same prescription.
Personalized practitioners order pharmacogenomic testing before prescribing medications for chronic conditions, then adjust doses or switch drug classes based on your genetic profile. This single intervention eliminates months or years of side effects, hospitalizations, and failed treatment attempts. Patients report feeling better within days of switching to genetically appropriate medications, experiencing improvements in energy, mood, and cognitive function that had nothing to do with the condition being treated but everything to do with drug toxicity from mismatched prescriptions.
Chronic Disease Management Becomes Predictable and Measurable
Chronic conditions like type 2 diabetes, heart disease, and autoimmune disorders respond to personalized intervention because the root causes vary dramatically between individuals. Two patients with identical type 2 diabetes diagnoses might have completely different biological drivers: one has insulin resistance from metabolic dysfunction, another from chronic inflammation, and a third from specific genetic variations affecting glucose regulation. Standard diabetes management prescribes metformin and lifestyle modification to both, hoping one of these approaches works.
Personalized practitioners order metabolic panels, inflammatory markers, and genetic testing to identify which mechanism dominates each patient’s condition, then prescribe interventions targeting that specific driver. The first patient receives targeted nutrition and insulin-sensitizing strategies, the second receives anti-inflammatory protocols, and the third receives medication matched to their genetic profile. Outcomes improve because treatment addresses actual biology rather than statistical averages. Patients achieve better glucose control with lower medication doses, experience sustained weight loss when interventions match their metabolic type, and avoid the progression to kidney disease or neuropathy that standard management often fails to prevent.
Longer Appointments Enable Thorough Treatment Planning
Longer appointment times in personalized care models enable practitioners to discuss findings thoroughly and build realistic treatment plans. Patients understand why their specific interventions matter for their unique biology rather than following generic recommendations that might not apply to them. This extended time transforms the conversation from a rushed checklist into a collaborative discussion about root causes, treatment options, and realistic expectations for health improvement.
Final Thoughts
Personalized healthcare represents a fundamental shift away from population-level protocols toward treatment tailored to your individual biology. Genetic testing, biomarker analysis, and advanced diagnostics reveal what makes your health unique, enabling practitioners to match interventions to your specific needs rather than applying standard formulas that work for some patients but fail for others. The evidence is clear: when treatment aligns with your genetic makeup and metabolic profile, outcomes improve, side effects diminish, and chronic conditions become manageable rather than progressive.
The healthcare industry is moving decisively in this direction. Investment in personalized medicine grew 53 percent between 2011 and 2015, and the global market for tailored treatment approaches is forecast to reach 715 billion dollars by 2026.
This growth reflects a simple reality: patients and practitioners alike recognize that one-size-fits-all medicine wastes resources and leaves people suffering unnecessarily. More than 2,600 Direct Primary Care practices now operate across the United States, many incorporating personalized approaches that traditional insurance-based medicine cannot support due to time and financial constraints.
Your personalized healthcare journey starts with finding a practitioner who invests time in understanding your unique biology rather than rushing through appointments constrained by insurance billing cycles. Visit NuMed DPC to explore how direct primary care can transform your health outcomes and empower you to take control of your medical journey.