Sleep problems affect millions of people, and many turn to natural remedies for relief. Progesterone plays a significant role in regulating sleep, yet many don’t understand how progesterone cream for sleep actually works or whether it truly helps.
At NuMed DPC, we’ve seen growing interest in topical progesterone as a potential sleep solution. This guide breaks down the science, safety, and realistic expectations around this approach.
How Progesterone Shapes Your Sleep
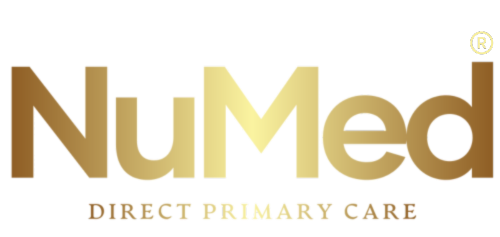
Progesterone acts as a natural sedative in your brain by enhancing GABA activity, the same neurotransmitter that calming medications target. This mechanism doesn’t just make you drowsy-it actively supports slow-wave sleep, the deep restorative stage where your brain consolidates memories and repairs tissue. Research from the National Library of Medicine shows that progesterone influences your nervous, cardiovascular, and thermoregulation systems simultaneously, meaning a decline in this hormone disrupts far more than just sleep onset.
The Steep Hormonal Decline During Perimenopause and Menopause
During perimenopause and menopause, progesterone drops earlier and more sharply than estrogen, which explains why many women experience sudden insomnia and night sweats despite feeling fine just months earlier. This hormonal shift is not gradual-it’s a steep decline that catches most women off guard. Standard sleep treatments often fail because they ignore the underlying hormonal cause.
Why Your Brain Loses Its Natural Sleep Signal
When progesterone levels fall, your brain loses its natural brake on wakefulness. You may wake at 3 a.m. drenched in sweat, or lie awake despite exhaustion because your nervous system lacks the chemical signal to stay asleep. The sleep disturbances you experience aren’t just about feeling tired; night sweats disrupt your sleep architecture, reducing the time spent in restorative sleep stages.
The Problem With Standard Sleep Interventions
Many women spend years taking antidepressants or over-the-counter sleep aids without addressing the hormonal imbalance driving their insomnia. Research published in MedlinePlus emphasizes that progesterone deficiency can coexist with other hormone imbalances and may be completely overlooked when treating sleep problems with only pharmaceutical sleep aids. The timing of progesterone supplementation matters significantly: taking it at night leverages its sedative effects for sleep onset and maintenance, while daytime doses cause drowsiness that interferes with productivity and alertness.
Dosing Matters More Than Most Realize
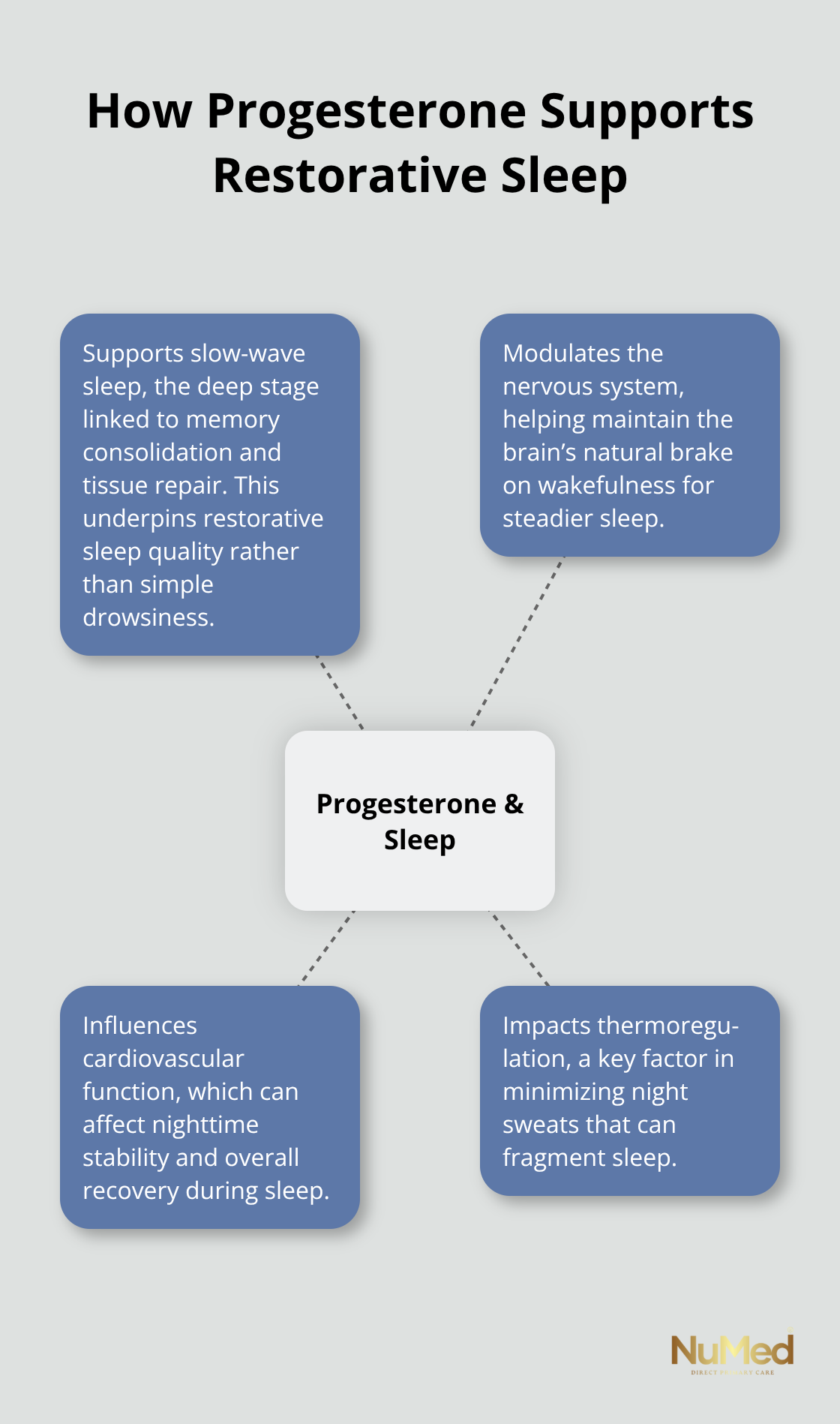
Low doses simply don’t work-proper dosing is essential for meaningful sleep improvement. Many over-the-counter creams deliver only 25 mg per pump, which proves ineffective for women with significant hormonal decline. Understanding whether topical progesterone cream can actually deliver adequate doses becomes the next critical question in determining whether this approach suits your individual situation.
Progesterone Cream as a Sleep Aid
How Topical Progesterone Reaches Your Bloodstream
Topical progesterone cream sounds appealing because it bypasses your digestive system, but the reality is far more complicated than most assume. When you apply progesterone cream to your skin, it must cross the stratum corneum and reach your bloodstream to produce systemic effects on sleep. The problem is that absorption rates vary dramatically depending on application site, formulation strength, and individual skin characteristics.
Over-the-counter progesterone creams typically deliver around 25 mg per pump, but studies show that standard OTC doses often prove inadequate for women experiencing significant hormonal decline during perimenopause and menopause. Many women find themselves applying four pumps per application just to reach therapeutic levels, making the process inconvenient and inconsistent. The wrist or bikini line are common application site because skin thickness affects penetration, yet even with optimal placement, absorption remains unpredictable.
Research published in the National Library of Medicine indicates that low progesterone doses simply don’t work for meaningful sleep improvement, which explains why countless women report no benefit from drugstore creams despite consistent use. This dosing limitation pushes many patients toward compounding pharmacies that can create higher-concentration formulations tailored to individual needs, typically ranging from 50 mg to 200 mg per application.
Timing Your Application for Maximum Sleep Benefit
Timing your application matters significantly-you should take progesterone at bedtime to leverage its sedative effects for sleep onset and maintenance. Morning application causes daytime drowsiness that interferes with alertness and productivity, making it counterproductive for most women. This simple timing adjustment can mean the difference between experiencing sleep improvement and wasting money on ineffective doses.
How Progesterone Cream Compares to Other Sleep Interventions
Standard sleep aids like benzodiazepines and over-the-counter antihistamines address symptoms without touching the underlying hormonal cause, which means they fail for women whose insomnia stems from progesterone deficiency. Antidepressants, often prescribed off-label for sleep, work through entirely different mechanisms and frequently miss the hormonal component driving nighttime wakefulness and night sweats.
Progesterone cream offers a fundamentally different approach because it targets the specific neurochemical deficit-enhanced GABA activity and slow-wave sleep support, rather than forcing sedation through unrelated pathways. However, progesterone cream works best as part of a broader hormonal strategy rather than in isolation. Many women experience superior sleep improvement when progesterone combines with balanced estrogen levels, since estrogen decline contributes significantly to vasomotor symptoms like night sweats that fragment sleep architecture.
Why Hormonal Balance Matters More Than Single Solutions
This means a single cream application may not solve your sleep problem if other hormonal imbalances remain unaddressed. Effective sleep management requires understanding your complete hormonal picture, not just selecting the most convenient topical option. Individual responses vary considerably-some women report easier sleep and fewer awakenings within days, while others require weeks of consistent use at proper doses before noticing improvement.
The Role of Blood Testing in Dosing Decisions
Starting with blood testing to measure your actual hormone levels allows for dosing decisions grounded in your specific situation rather than guesswork. Testing hormone levels in the first half of your cycle (when progesterone is low) helps tailor therapy to mimic natural levels with replacement. This approach ensures that if you choose topical progesterone, you’re using a dose likely to produce meaningful results rather than relying on standard OTC recommendations that may not fit your individual needs. Understanding your baseline hormone status becomes the foundation for determining whether progesterone cream alone will address your sleep disturbances or whether additional hormonal support is necessary.
Safety and Side Effects You Need to Know
Progesterone cream produces real effects in your body, which means real side effects are possible. According to MedlinePlus, common adverse effects include headache, breast tenderness, upset stomach, vomiting, diarrhea, constipation, fatigue, and mood changes. More concerning, some women experience irritability, agitation, or depression when progesterone levels climb too high, a problem more common with pills or lozenges but possible with topical applications if dosing exceeds your tolerance. When progesterone combines with estrogen therapy, the risks expand: research shows increased risk of heart attack, stroke, blood clots, and breast cancer, along with a documented association between progestin and estrogen use and elevated dementia risk.
Serious Side Effects That Demand Immediate Attention
Serious side effects require immediate medical attention. These include sudden severe headache, sudden vision changes, chest pain, coughing up blood, and severe shortness of breath.
Your individual risk profile matters enormously-women with a history of blood clots, stroke, heart disease, or certain cancers face substantially different risk calculations than others. Before starting topical progesterone, tell your healthcare provider about all medications and supplements you take, including St. John’s wort, which can interact with progesterone. Grapefruit juice also interacts with progesterone metabolism, so check with your provider about dietary restrictions.
Dosing Strategy That Actually Works
Standard OTC doses fail most women because 25 mg per pump simply doesn’t produce measurable changes in sleep architecture. Proper dosing requires individual assessment rather than relying on package directions. Many women need 50 to 200 mg per application to achieve therapeutic effects, which means compounding pharmacies often provide better results than drugstore options. Apply progesterone at bedtime consistently, ideally to areas with thinner skin like the wrist or inner bikini line, where absorption improves. Four pumps of standard cream per application becomes tedious and encourages inconsistency, which sabotages results-another reason higher-concentration formulations from compounding pharmacies make practical sense.
Timing and Consistency Matter for Safety and Efficacy
Taking progesterone at the same time each evening helps you maintain stable hormone levels and remember your dose, but daytime doses cause drowsiness that interferes with work and alertness. If progesterone causes dizziness or drowsiness initially, take it exclusively at bedtime and avoid driving until you know your response. If you plan surgery or extended bed rest, progesterone therapy often needs to stop several weeks beforehand to reduce clotting risk.
When Professional Guidance Becomes Essential
Testing hormone levels in the first half of your menstrual cycle provides the baseline needed to make intelligent dosing decisions rather than guessing. If you experience sleep disturbances alongside hot flashes, night sweats, mood instability, or vaginal dryness, a hormonal assessment should precede any topical cream purchase. Your healthcare provider needs to know whether you’re pregnant, planning pregnancy, or breastfeeding before progesterone therapy begins, since implications exist for each situation. If sleep problems persist despite progesterone use at proper doses for four to six weeks, or if side effects emerge that concern you, contact your provider rather than self-adjusting your approach. Women taking multiple psychiatric medications who still struggle with insomnia particularly benefit from hormonal evaluation, since progesterone deficiency frequently coexists with other imbalances that medications alone won’t address. Insurance coverage for hormone testing varies considerably, but scheduling an evaluation with a healthcare provider familiar with hormone assessment can clarify your options without unnecessary delay.
Final Thoughts
Progesterone cream for sleep works best when you base your approach on realistic expectations and individual assessment rather than hope that a topical application will solve complex hormonal disruption. The evidence shows that progesterone influences sleep through measurable neurochemical pathways, enhancing GABA activity and supporting deep restorative sleep stages. However, this doesn’t mean every woman experiences dramatic improvement, and standard over-the-counter doses won’t produce meaningful results for most people experiencing significant hormonal decline.
Your individual response depends on multiple factors: your actual hormone levels, the dose you’re using, whether other hormonal imbalances exist alongside progesterone deficiency, and your overall health status. Some women report easier sleep and fewer awakenings within days of starting properly dosed progesterone cream, while others require weeks of consistent use before noticing changes. A small percentage experience no benefit regardless of dosing, which is why blood testing before starting therapy matters so much.
Effective sleep management rarely involves a single solution, and if progesterone deficiency drives your insomnia, addressing it makes sense. If night sweats fragment your sleep, balancing both progesterone and estrogen typically produces better results than progesterone alone. At NuMed DPC, we focus on addressing root causes rather than treating symptoms in isolation, which means comprehensive hormone assessment, proper dosing based on your individual needs, and ongoing monitoring to verify your approach actually works.