Hormonal imbalances affect millions of women, causing fatigue, mood swings, irregular cycles, and weight fluctuations that disrupt daily life. The good news is that female hormones respond well to natural interventions through diet, lifestyle, and environmental changes.
At NuMed DPC, we believe in addressing hormonal health at its root rather than masking symptoms. This guide walks you through proven strategies to support your body’s natural hormone regulation.
What’s Actually Causing Your Hormonal Imbalance
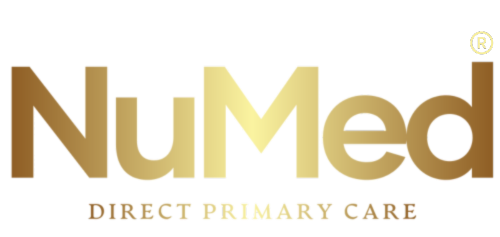
Hormonal imbalance doesn’t appear out of nowhere. Women experience disruptions across five critical hormones-cortisol, estrogen, progesterone, thyroid hormones, and insulin-and identifying what triggered the imbalance matters far more than treating symptoms alone. Chronic stress elevates cortisol, which suppresses progesterone and disrupts your menstrual cycle.
Thyroid dysfunction directly impacts metabolism and mood, with hypothyroidism affecting approximately 5% of the general population. PCOS affects 5%-18% of reproductive-age women and causes insulin resistance that blocks ovulation. Poor sleep quality reduces melatonin production and increases cortisol, creating a vicious cycle that worsens fatigue and weight gain around the midsection. Endocrine-disrupting chemicals in plastics, certain cosmetics, and household products actively interfere with hormone signaling, so exposure reduction isn’t optional if you’re serious about balance.
Recognizing Symptoms Before They Worsen
The symptoms you’re experiencing aren’t random. Persistent fatigue combined with brain fog signals low thyroid function or elevated cortisol. Irregular or heavy periods with severe PMS indicate progesterone deficiency or estrogen dominance. Night sweats and sleep disturbances during perimenopause reflect declining estrogen and progesterone. Stubborn weight gain concentrated in your belly points to insulin resistance or cortisol dysregulation. Hair loss, acne, or low libido suggest testosterone or thyroid imbalances. Early intervention prevents cascading problems-addressing hormonal disruption at the symptom stage stops progression into insulin resistance, osteoporosis risk, autoimmune flares, or postmenopausal heart disease. Waiting for symptoms to worsen guarantees more complex treatment later.
Why Lab Testing Reveals Root Causes
A comprehensive hormone evaluation through labs measuring TSH, T3, T4, estrogen, progesterone, testosterone, cortisol, DHEA, insulin, glucose, and vitamin D reveals root causes rather than guessing which hormone needs support. This lab-informed approach means you’re not applying quick fixes that fail within months. Your practitioner can determine whether your symptoms stem from thyroid dysfunction requiring medication adjustment, PCOS needing targeted supplementation, adrenal exhaustion from chronic stress, or a combination requiring integrated treatment.
Professional Assessment Distinguishes Real Imbalances from Normal Aging
Hormonal symptoms often masquerade as normal aging or stress, which is why distinguishing underlying imbalances from lifestyle factors requires professional guidance. A direct primary care model provides longer appointment times and direct doctor access, allowing thorough investigation of your specific hormonal picture. The difference between receiving a personalized, lab-informed plan versus generic advice determines whether you experience meaningful improvement in energy, mood, sleep, and quality of life within three to six months or continue struggling for years. Understanding your hormonal foundation through professional assessment positions you to select the right interventions-whether dietary changes, lifestyle modifications, supplements, or medical treatment-that actually work for your body.
What You Should Actually Eat to Balance Your Hormones
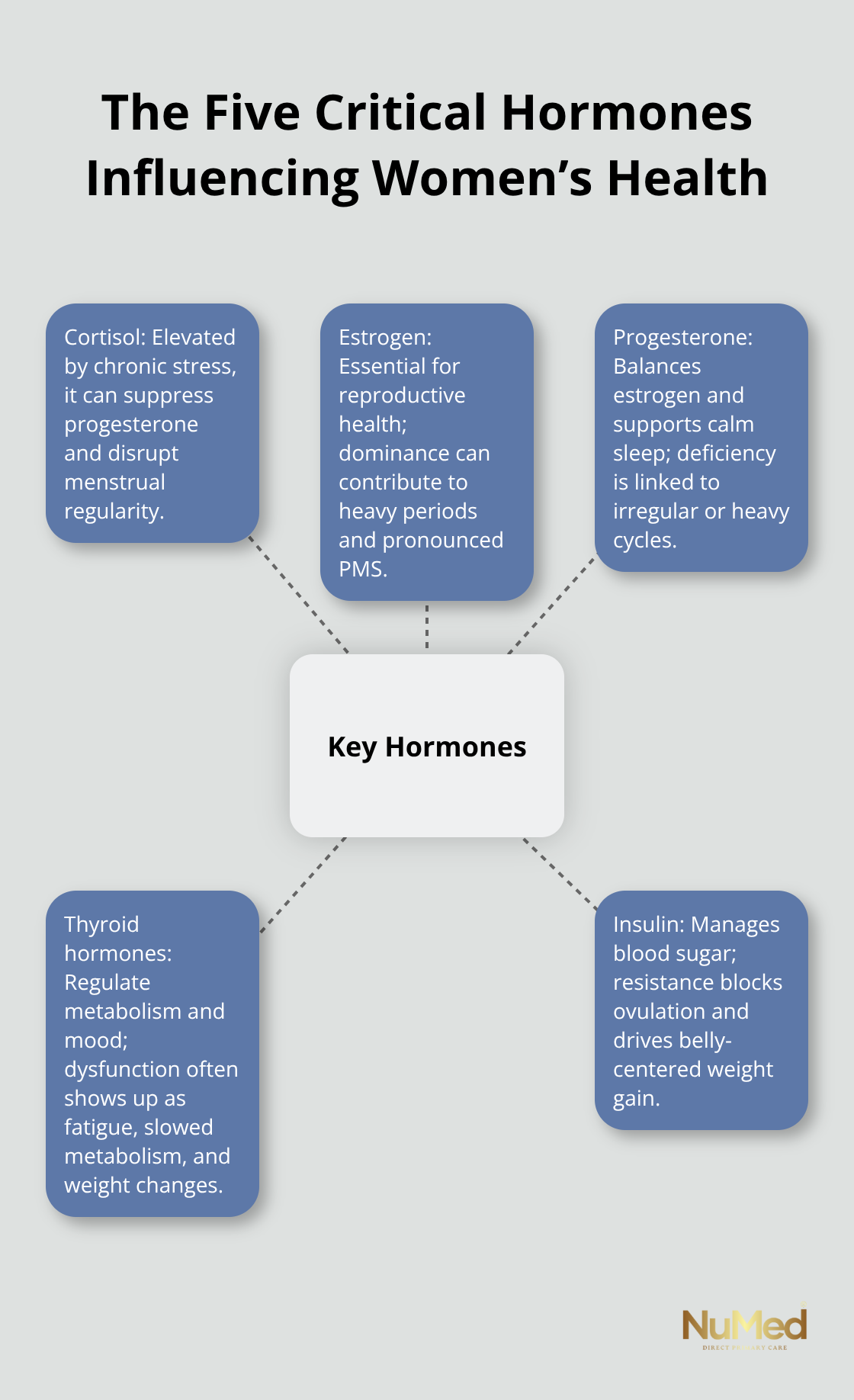
The food you eat directly controls hormone production, and this is where most women make critical mistakes. You cannot out-supplement a poor diet, and generic nutrition advice fails because hormonal needs change across your menstrual cycle, perimenopause, and menopause. Your estrogen and progesterone depend on adequate unsaturated fats, sufficient protein intake, and fiber from whole foods. Women who chronically undereat, a pattern research shows affects approximately 40% of women trying to lose weight, suppress estrogen, progesterone, LH, and FSH production, triggering irregular cycles and worsening fatigue. Omega-3 fatty acids from salmon, sardines, walnuts, and chia seeds reduce inflammation that exacerbates hormonal symptoms. Vitamin D supports sex hormone health and fertility, yet approximately 40% of Americans have insufficient vitamin D levels according to research from Boston University. Include fatty fish, egg yolks, and fortified foods regularly, or discuss supplementation with your healthcare provider if blood work shows a deficiency. Magnesium-rich foods like pumpkin seeds, almonds, spinach, and black beans directly reduce PMS severity and support sleep quality, which regulates cortisol and melatonin. Try 310–320 mg daily for women, though many consume only 200 mg. Phytoestrogens from flaxseeds, chickpeas, and lentils provide plant compounds that gently support estrogen balance during perimenopause without the risks of synthetic hormones.
Stabilize Blood Sugar to Prevent Hormonal Chaos
Insulin resistance drives hormonal chaos more than most women realize. When blood sugar spikes, your pancreas releases excess insulin, which increases androgen production and blocks ovulation-this is why PCOS and insulin resistance travel together. Prevent this by combining protein, healthy fats, and fiber in every meal. An apple with almond butter, eggs with cheese and spinach on whole-grain toast, or a curry with chickpeas and vegetables all stabilize blood sugar across three to four hours. Avoid extreme low-carb dieting because your body needs carbohydrates for hormone production. Women who restrict carbs below 100 grams daily often experience worsening fatigue, irregular cycles, and lower progesterone. Processed foods, refined sugars, and seed oils (canola, soybean, sunflower) promote inflammation that worsens cortisol dysregulation and estrogen dominance. These oils appear in 95% of packaged foods, so reading labels matters. Alcohol and excessive caffeine elevate cortisol and interfere with sleep quality, which then destabilizes all five critical hormones.
If you drink daily, reducing to three days weekly shows measurable improvements in sleep architecture and morning cortisol levels within two weeks.
Support Your Thyroid with Essential Nutrients
Your thyroid hormones control metabolism, mood, and energy, yet iodine deficiency remains common even in developed countries. Iodized salt, dairy products, and nori seaweed provide iodine, but you need only 150 micrograms daily; excessive iodine actually worsens thyroid function. Iron, zinc, selenium, and vitamin B12 are equally critical because your thyroid cannot produce hormones without them. Legumes, animal proteins, broccoli, and whole grains provide iron and zinc. Eggs and whole grains supply selenium. Animal proteins and fortified foods cover B12, especially important if you avoid animal products. Eat adequate calories so your body has fuel for metabolism-this prevents the metabolic slowdown that occurs when undereating triggers thyroid hormone conversion problems. These nutritional foundations set the stage for understanding how sleep and stress management amplify or undermine your dietary efforts.
How Sleep and Stress Control Your Hormones
Sleep deprivation sabotages hormonal balance faster than almost any other factor, yet most women accept five to six hours nightly as normal. Your cortisol, melatonin, and growth hormone synchronize to a 24-hour rhythm, and disrupting this rhythm triggers cascading hormonal failures. Keep your bedroom temperature at 65°F because your core body temperature must drop 2-3°F to initiate sleep onset. Moisture-wicking sleepwear prevents night sweats from disrupting your sleep architecture. Magnesium glycinate at 300-400 mg taken two hours before bed reduces racing thoughts and supports sleep quality without the next-day grogginess that comes from standard magnesium or melatonin supplements. If you wake during the night, avoid clock-watching because monitoring time triggers cortisol spikes that prevent returning to deep sleep.
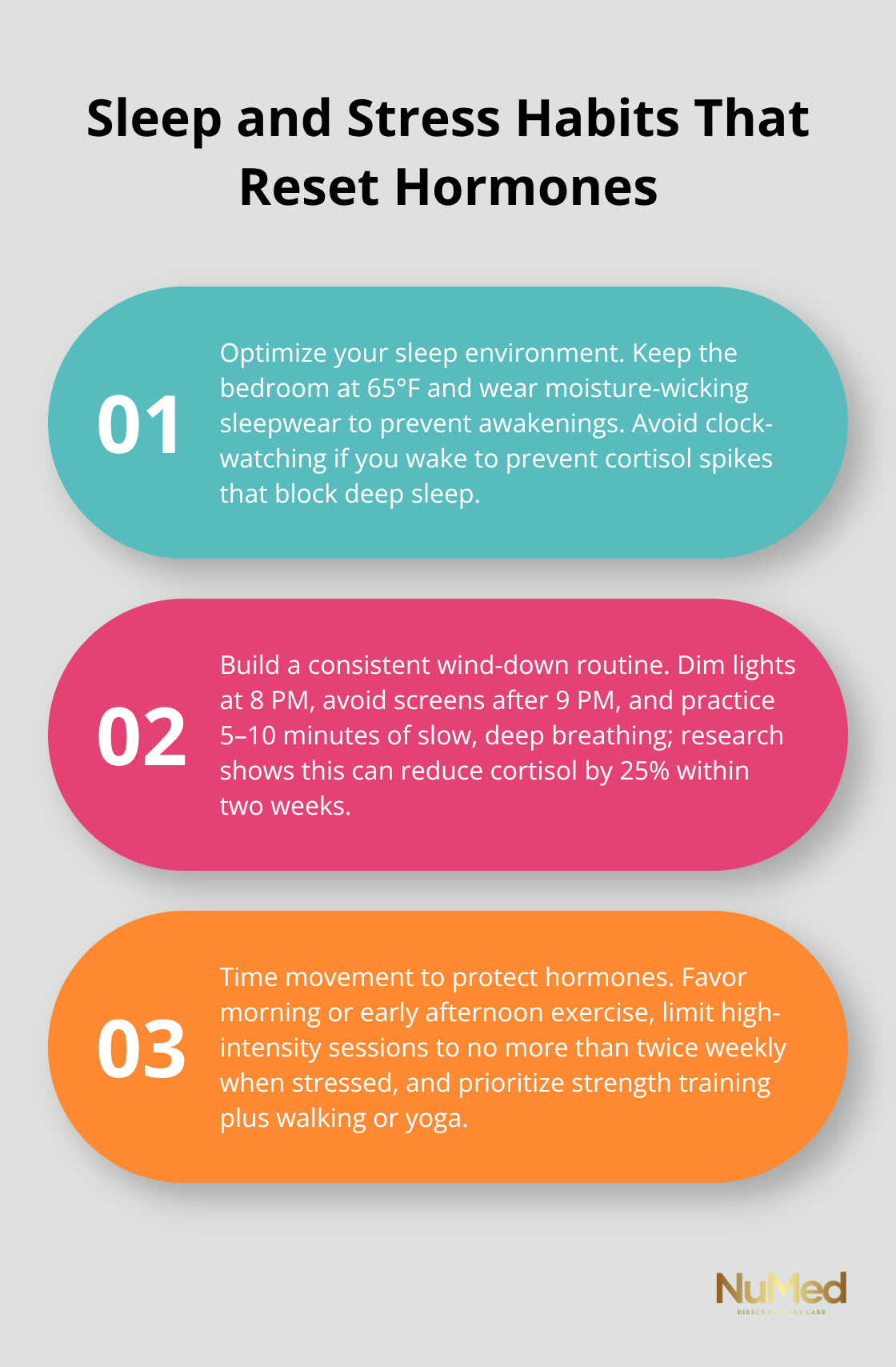
Establish a 30-minute wind-down routine starting at the same time each evening-this consistency trains your nervous system to recognize the sleep signal. Dim lights at 8 PM, avoid screens after 9 PM, and practice 5-10 minutes of deep breathing because slow exhales activate your parasympathetic nervous system and lower cortisol before bed. Research from the University of California shows that even 10 minutes of daily breathing exercises reduces cortisol by 25% within two weeks, and this effect compounds over months.
How Cortisol Dysregulation Drives Weight Gain and Hormonal Chaos
Chronic stress elevates cortisol, which directly suppresses progesterone production and triggers weight gain, particularly in the face and abdomen. Stress management isn’t optional meditation, or yoga-it’s a medical necessity for hormonal recovery. Mindfulness practice for 10-15 minutes daily reduces cortisol and increases DHEA, your anti-aging hormone, according to studies from Johns Hopkins Medicine. If meditation feels abstract, start with body scans where you mentally check each body part from toes to head, spending 20 seconds on each area and noticing tension without judgment.
Movement Timing and Type Matter More Than Intensity
Walking outdoors for 20-30 minutes at a moderate pace reduces cortisol more effectively than gym workouts because natural light exposure resets your circadian rhythm while movement activates parasympathetic calm. High-intensity exercise actually worsens cortisol if performed more than twice weekly when you’re already stressed, so prioritize strength training 2-3 times per week combined with walking, yoga for balance, or water-based exercise if joint pain limits impact activities. The timing matters-exercise in the morning or early afternoon hours because evening workouts elevate cortisol and disrupt sleep.
Eliminate Hidden Hormone Disruptors in Your Environment
Environmental toxins from plastics containing BPA, phthalates in fragranced products, and pesticides in non-organic produce actively mimic hormones and block receptor sites. Switch to glass or stainless steel containers, choose fragrance-free personal care products, and purchase organic for the Dirty Dozen produce list. These changes remove exposures that sabotage your dietary and lifestyle efforts.
Final Thoughts
Balancing female hormones naturally requires you to address diet, sleep, stress, and environmental exposures simultaneously rather than fixing one area while neglecting others. The strategies outlined here work because they target root causes instead of masking symptoms. Consistent dietary choices that stabilize blood sugar, adequate sleep that resets your circadian rhythm, stress management that lowers cortisol, and movement that supports your nervous system create the foundation for sustainable hormone balance.
Knowing what to do and executing a personalized plan presents different challenges. If you’ve tried dietary changes and lifestyle modifications without improvement, or if your symptoms suggest thyroid dysfunction, PCOS, or adrenal exhaustion, professional assessment becomes necessary. A healthcare provider can order comprehensive labs measuring your thyroid hormones, sex hormones, cortisol, insulin, and vitamin D to identify exactly which hormonal systems need support.
We at NuMed DPC address hormonal health through personalized evaluation and integrated treatment combining functional medicine, targeted supplementation, and lifestyle coaching. Our direct primary care model provides longer appointment times and direct doctor access, allowing thorough investigation of your hormonal picture rather than rushed consultations. Contact us today to schedule your comprehensive hormone evaluation and start your personalized plan for natural female hormone balance.