Starting a Direct Primary Care (DPC) practice can be a game-changing decision for healthcare providers. At NuMed DPC, we’ve seen firsthand how this model revolutionizes patient care and physician satisfaction.
This guide will walk you through the essential steps on how to start a Direct Primary Care practice, from understanding the core principles to navigating legal considerations and setting up your clinic. We’ll share practical insights to help you transition smoothly into this innovative healthcare model.
What Is Direct Primary Care?
A Revolutionary Healthcare Model
Direct Primary Care (DPC) transforms the healthcare landscape by removing insurance companies from the primary care equation. Patients pay a monthly or annual fee directly to their healthcare provider for a wide range of primary care services.
Smaller Patient Panels, Personalized Care
DPC physicians typically manage a patient panel of about 400 to 600 individuals, compared to 2,000–2,500 in traditional practices. This reduction allows for longer appointments (30 to 60 minutes) instead of the standard 15-minute slots. The Journal of the American Board of Family Medicine reports that DPC physicians spend 85.6% of their time in direct patient care activities, versus 59.1% in traditional practices. This increase in face-time promotes better health outcomes and higher satisfaction for both doctors and patients.
Financial Advantages
DPC offers financial benefits to patients and physicians alike. Patients often reduce their out-of-pocket healthcare costs. A 2020 survey by the Direct Primary Care Coalition revealed that DPC members saved 30-50% on healthcare expenses compared to those using traditional insurance-based primary care.
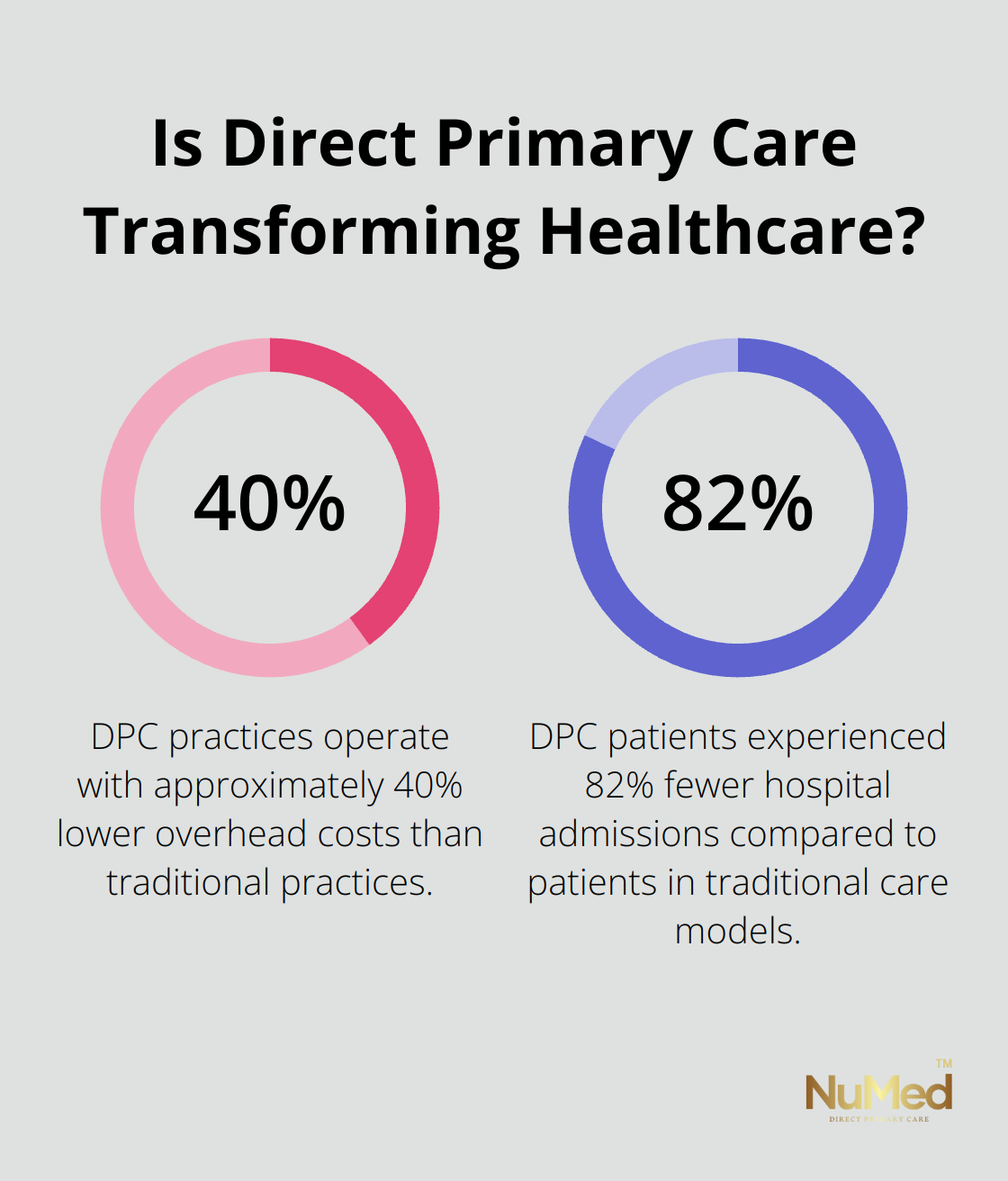
Physicians can increase their income and reduce overhead costs through the DPC model. The elimination of insurance billing staff and reduced administrative burdens allows DPC practices to operate with approximately 40% lower overhead costs than traditional practices (according to data from the American Academy of Family Physicians).
Enhanced Accessibility and Care Quality
DPC significantly improves access to care. Many practices offer same-day or next-day appointments, 24/7 physician access via phone or text, and in some cases, house calls. This level of accessibility addresses health issues promptly, preventing escalation into more serious conditions.
A 2018 study in the Journal of American Physicians and Surgeons found that DPC patients experienced 82% fewer hospital admissions compared to patients in traditional care models. This reduction in hospitalizations not only improves patient health but also contributes to overall healthcare cost savings.
Complementing Health Insurance
It’s important to note that DPC does not replace health insurance. Patients should maintain a high-deductible health plan for catastrophic events or specialized care outside primary care scope. However, for daily health needs and chronic disease management, DPC provides a cost-effective and patient-centered approach that continues to gain popularity across the United States.
As we move forward, we’ll explore the legal and financial considerations essential for starting your own DPC practice. These factors play a critical role in establishing a successful and compliant healthcare business.
Legal and Financial Essentials for Your DPC Practice
Selecting the Right Business Structure
The selection of an appropriate business structure stands as a critical first step in establishing a Direct Primary Care (DPC) practice. The first official step in opening your practice is to create a legal entity. The regulations surrounding this process vary by state. Most DPC practices choose either a Limited Liability Company (LLC) or Professional Corporation (PC). An LLC provides flexibility and personal asset protection, while a PC caters specifically to licensed professionals.
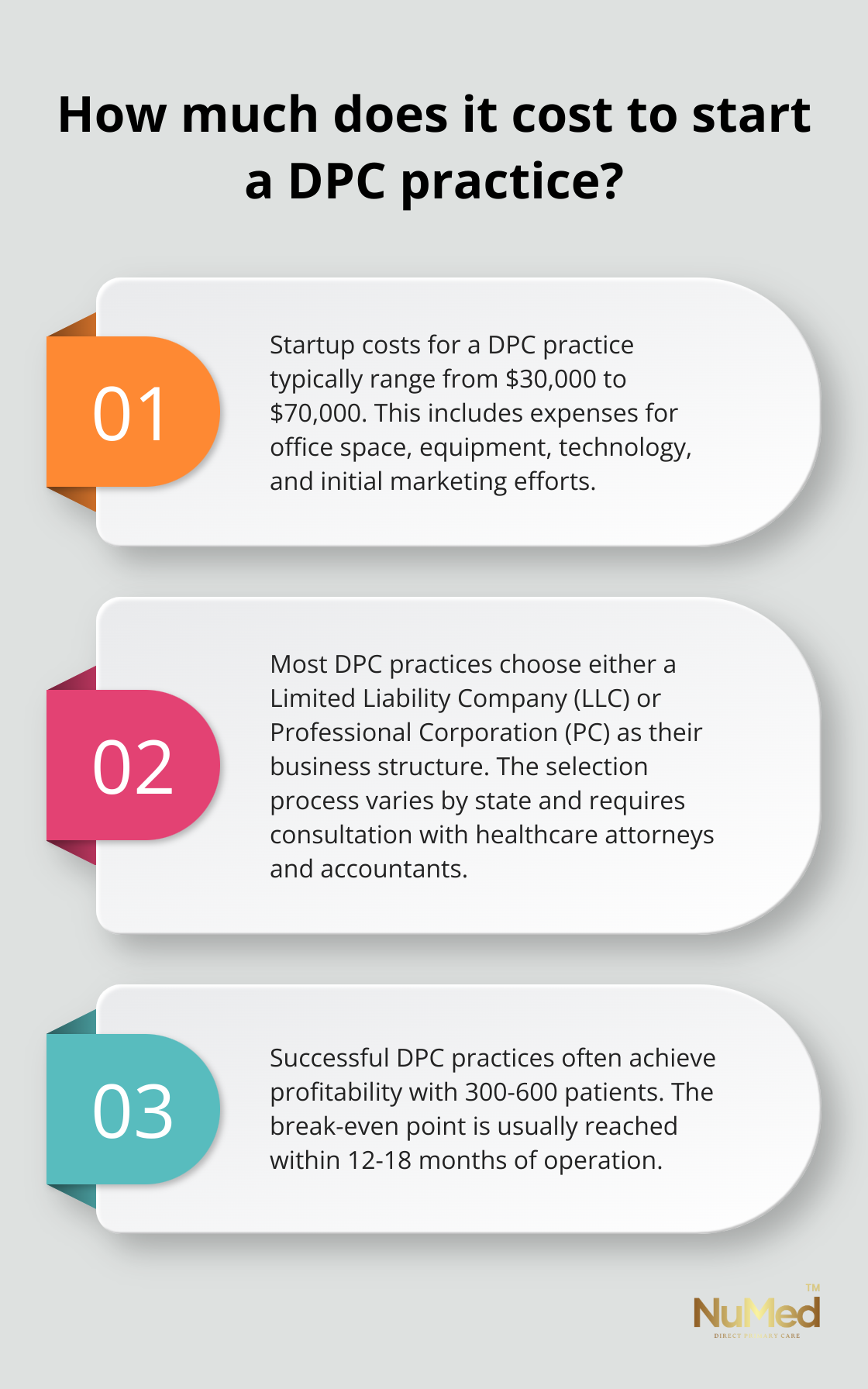
A healthcare attorney and accountant can offer valuable guidance in determining the best structure for your specific situation. They will analyze the pros and cons of each option, taking into account factors such as liability protection, tax implications, and future growth plans.
Creating a Robust Financial Plan
The development of a comprehensive financial plan proves essential for the long-term success of your DPC practice. Begin by estimating your startup costs, which typically fall between $30,000 and $70,000 (according to the DPC Alliance). These costs encompass office space, equipment, technology, and initial marketing efforts.
Next, project your monthly expenses and revenue. Factor in rent, utilities, staff salaries, and supplies. For revenue, determine your membership fees and target patient panel size. DPC offers a transparent pricing model, with a flat monthly fee covering most primary care services. This simplicity and predictability make healthcare more accessible.
Try to reach a break-even point within 12-18 months. Many successful DPC practices achieve profitability with 300-600 patients, depending on their fee structure and overhead costs.
Navigating Regulatory Compliance
The understanding and adherence to regulatory requirements play a vital role in operating a compliant DPC practice. Key areas of focus include:
- HIPAA Compliance: Meet all HIPAA requirements for patient privacy and data security. Implement robust systems and provide thorough staff training.
- State Regulations: DPC laws vary by state. Some states have enacted specific DPC legislation, while others regulate it under existing insurance laws. Research your state’s requirements and consider joining state-level DPC associations for guidance.
- Medicare Opt-Out: If you plan to see Medicare patients, you must formally opt-out of Medicare. This process requires renewal every two years.
- Business Licensing: Obtain all necessary local and state business licenses. Requirements vary by location, so check with your local chamber of commerce or small business administration.
- Malpractice Insurance: While DPC practices often face fewer malpractice claims, insurance remains essential. Look for policies tailored to DPC models, which can offer more cost-effective coverage than traditional malpractice insurance.
The establishment of a strong legal and financial foundation sets the stage for a successful DPC practice. As you move forward in your planning process, the next step involves the practical aspects of setting up your physical practice space and implementing the necessary systems to support your operations.
Setting Up Your DPC Practice Space
Location Selection
Choose a location that provides easy access for your target patient demographic. Consider factors such as parking availability, public transportation access, and proximity to complementary healthcare services. A centrally located office in a medical complex or busy commercial area can increase visibility and patient convenience.
Office Design
Try to create a warm and welcoming atmosphere that reflects your practice philosophy. Incorporate comfortable seating, natural lighting, and calming colors to reduce patient anxiety. Ensure your waiting area is spacious enough to maintain privacy and comfort, even during busy periods.
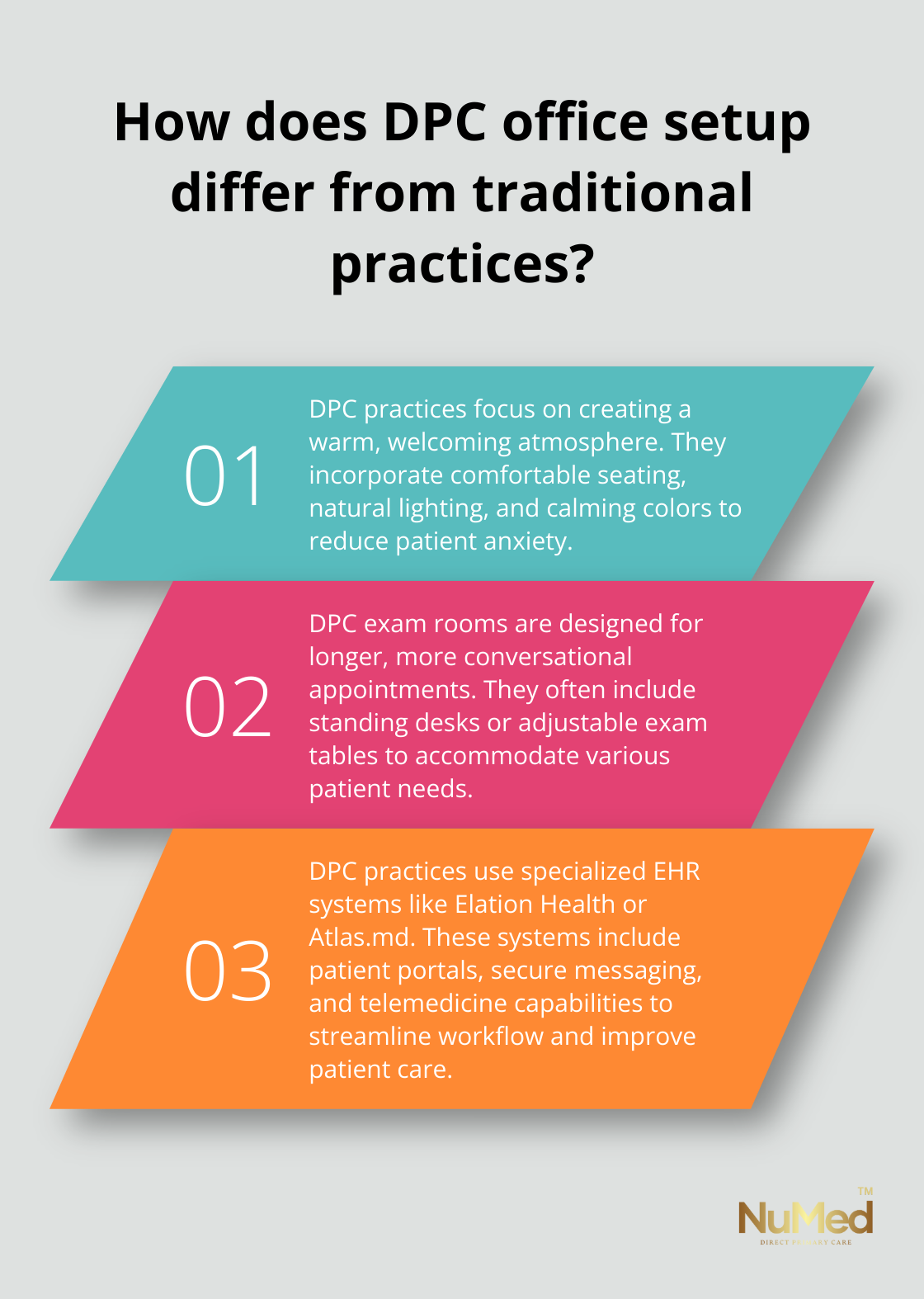
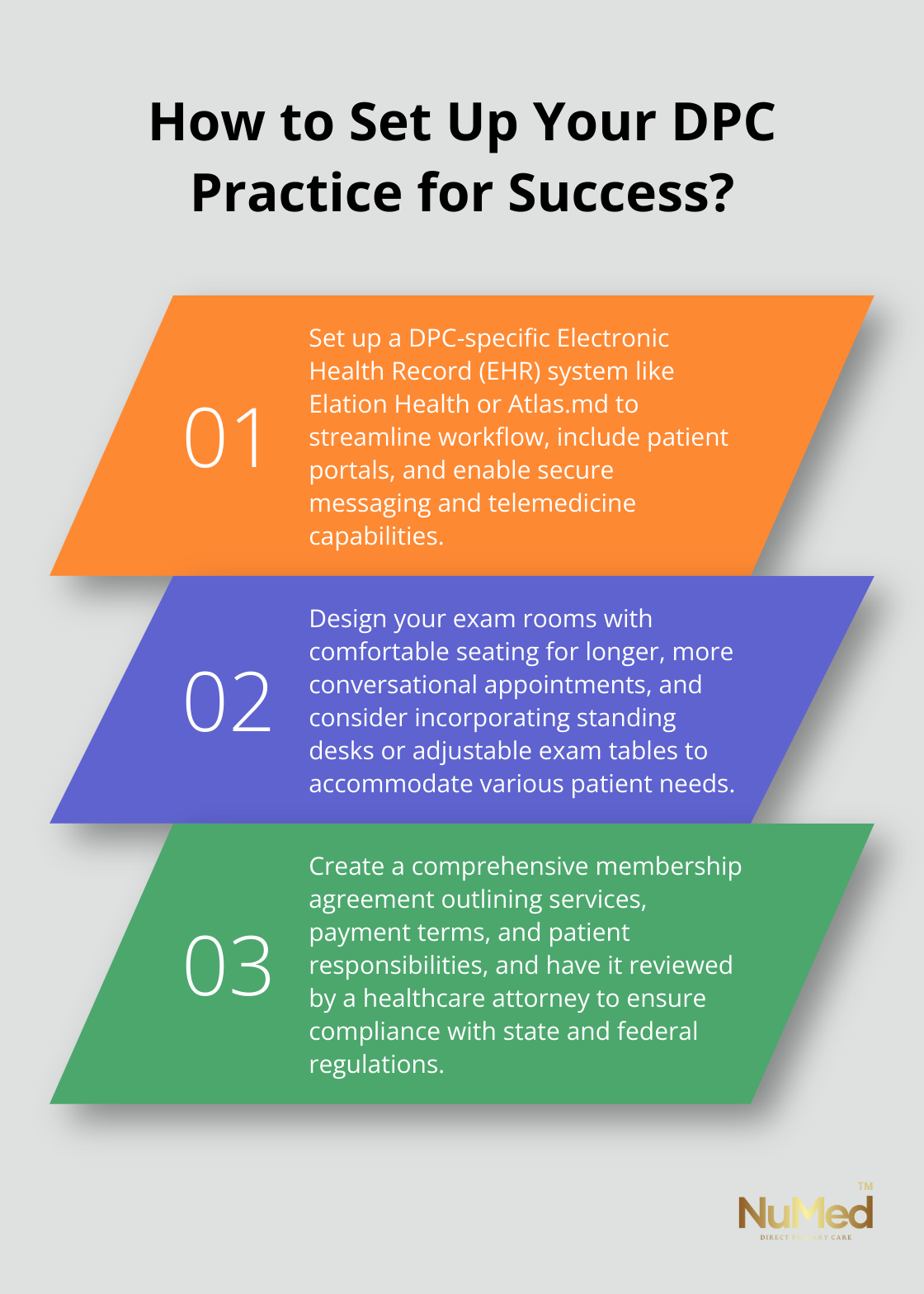
Design your exam rooms to facilitate meaningful patient interactions. Include comfortable seating for both you and your patients, as DPC appointments tend to be longer and more conversational than traditional primary care visits. Consider incorporating standing desks or adjustable exam tables to accommodate various patient needs and preferences.
Technology Implementation
Invest in the right technology to run an efficient DPC practice. Electronic Health Record (EHR) systems designed specifically for DPC practices (such as Elation Health or Atlas.md) can streamline your workflow and improve patient care. These systems often include features like patient portals, secure messaging, and telemedicine capabilities, which are particularly valuable in the DPC model.
Implement a robust practice management system to handle membership billing, appointment scheduling, and patient communication. Many DPC-specific platforms offer integrated solutions that combine EHR and practice management functionalities.
Invest in high-quality telemedicine equipment to provide virtual consultations. This may include high-resolution cameras, quality microphones, and reliable internet connectivity. Telemedicine interventions have shown significant improvements in patient health outcomes and cost savings.
Policies and Procedures
Develop clear policies and procedures to ensure smooth operations and maintain high-quality patient care. Start by creating a comprehensive membership agreement that outlines the services included in your DPC model, payment terms, and patient responsibilities. This agreement should be reviewed by a healthcare attorney to ensure compliance with state and federal regulations.
Establish protocols for after-hours care, prescription refills, and referrals to specialists. Clearly communicate these procedures to your patients to set appropriate expectations and minimize misunderstandings.
Implement a system for continuous quality improvement. Regularly solicit patient feedback through surveys or focus groups, and use this information to refine your processes and enhance patient satisfaction. Direct Primary Care practices often have reduced patient-to-doctor ratios compared to conventional fee-for-service settings, which can lead to improved patient care and satisfaction.
Final Thoughts
Starting a Direct Primary Care (DPC) practice transforms healthcare delivery and requires careful planning. You will face challenges such as building a patient base and educating potential members about the DPC model. The future of DPC looks promising, with the model gaining traction across the United States and the potential to significantly impact healthcare.
We at NuMed Primary Care have experienced the positive impact of the DPC model on both patients and practitioners. Our approach focuses on preventing illness, addressing root causes, and fostering strong patient-practitioner relationships. We offer comprehensive services including extensive lab work, functional medicine, and health coaching.
You have the power to make a lasting difference in your community’s health and well-being when you start a Direct Primary Care practice. You will revolutionize healthcare delivery by prioritizing the doctor-patient relationship and focusing on preventive care. The rewards of starting a DPC practice are significant and will benefit both you and your patients.