Bioidentical hormones have gained popularity as a treatment option for various hormonal imbalances. At NuMed DPC, we often receive questions about the pros and cons of bioidentical hormone therapy.
This blog post will explore the potential benefits and risks associated with these hormones, helping you make an informed decision about your health. We’ll dive into the science behind bioidentical hormones and discuss their impact on menopausal symptoms, bone health, and overall well-being.
What Are Bioidentical Hormones?
Definition and Composition
Bioidentical hormones are chemically the same as those the body makes. These hormones originate from plant sources (such as soy and yams) and undergo chemical alteration in a laboratory to match the molecular structure of human hormones.
The Science Behind Bioidentical Hormones
Scientists introduced the concept of bioidentical hormones in the 1930s as a potential alternative to synthetic hormone treatments. Unlike synthetic hormones, which have a slightly different molecular structure, bioidentical hormones are designed to be identical to those produced by our bodies. This structural similarity aims to result in fewer side effects and better overall tolerability.
Types of Bioidentical Hormones
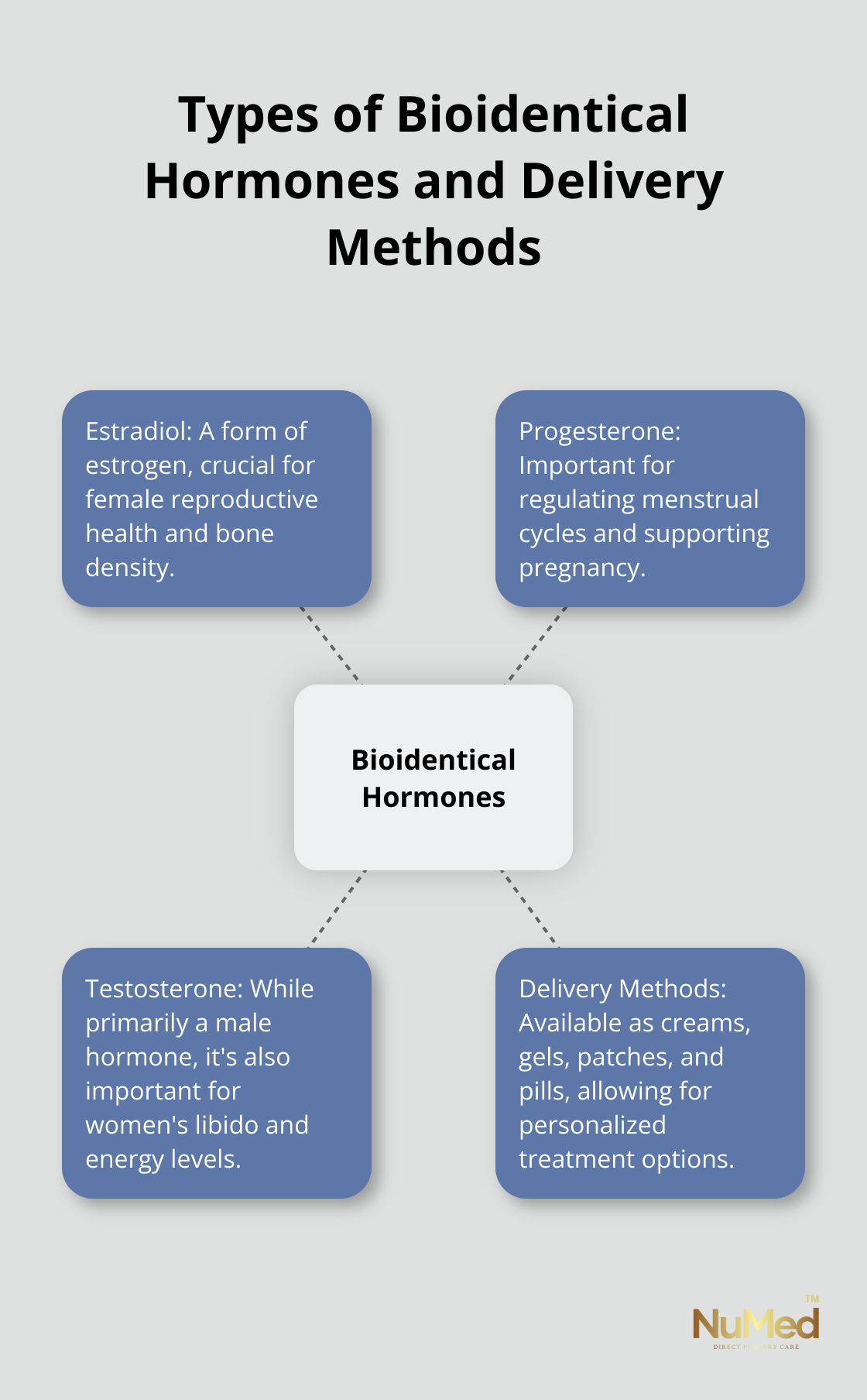
The most common bioidentical hormones used in therapy include:
- Estradiol
- Progesterone
- Testosterone
These hormones come in various forms, such as creams, gels, patches, and pills. The choice of delivery method often depends on the specific hormone and the patient’s individual needs.
Bioidentical vs. Synthetic Hormones
The main difference between bioidentical and synthetic hormones lies in their molecular structure. Synthetic hormones, while similar to natural hormones, have slight structural differences that can affect how they interact with the body. For example, the synthetic progestin used in many conventional hormone therapies has a different molecular structure than natural progesterone, which may lead to different effects and side effects.
A study published in the Journal of Clinical Endocrinology & Metabolism found that bioidentical progesterone may confer a lower risk of breast cancer than progestins. However, more research is needed to fully understand the long-term effects and safety profile of bioidentical hormones.
Availability and Regulation
Bioidentical hormones are available through various channels, including compounding pharmacies and FDA-approved formulations. It’s important to note that while some bioidentical hormones are FDA-approved, others (particularly those from compounding pharmacies) may not undergo the same rigorous testing and quality control.
Healthcare providers must carefully consider the source and quality of bioidentical hormones when prescribing them to patients. The regulation and oversight of these hormones continue to evolve as more research emerges about their efficacy and safety.
As we explore the potential benefits of bioidentical hormone therapy in the next section, it’s essential to understand that individual responses can vary. A thorough discussion with a qualified healthcare provider is necessary to determine the most appropriate treatment plan based on specific health needs and risk factors.
How Bioidentical Hormones Can Benefit You
Relief from Menopausal Symptoms
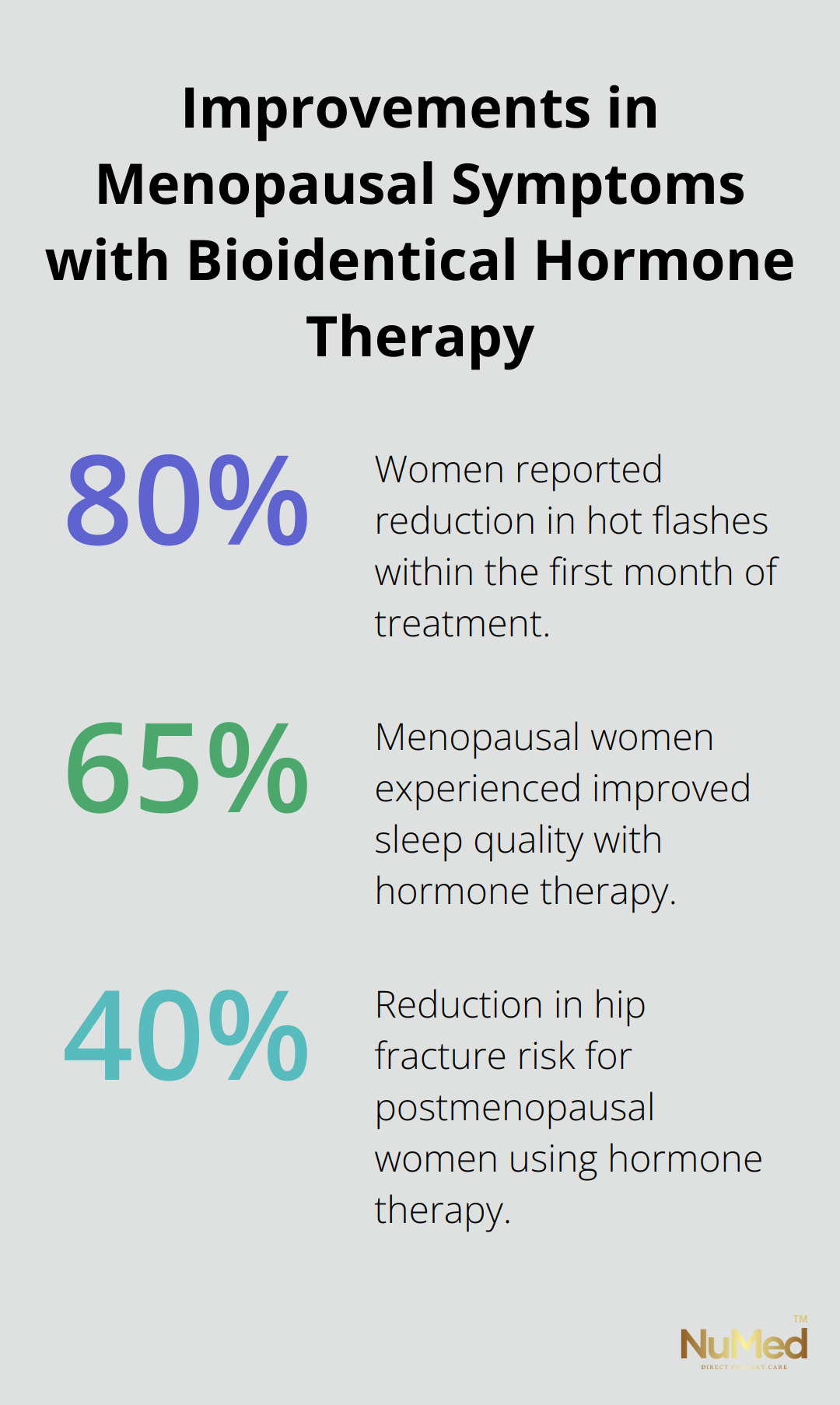
Hormone replacement therapy (HRT) replenishes women with ovarian hormones diminished during the natural menopausal transition to alleviate associated symptoms. Many women find relief from common menopausal symptoms through HRT. Hot flashes, night sweats, and vaginal dryness often improve with estrogen therapy. A study published in the Journal of Women’s Health found that 80% of women using bioidentical hormones reported a reduction in hot flashes within the first month of treatment.
Improved Bone Health
Osteoporosis presents a significant concern for postmenopausal women. Estrogen therapy shows promise in maintaining bone density. Research from the National Osteoporosis Foundation indicates that hormone therapy can reduce the risk of hip fractures by up to 40% in postmenopausal women (a statistic that underscores the potential impact of HRT on bone health).
Enhanced Mood and Cognitive Function
Hormonal fluctuations during menopause can lead to mood swings and cognitive changes. HRT may help stabilize mood and improve mental clarity. A study found that among non-carriers, current MHT use lowered the risk of cognitive impairment by almost half compared to never-users.
Potential Cardiovascular Benefits
Some research suggests that HRT might offer cardiovascular benefits, particularly when started early in menopause. A study published in the New England Journal of Medicine found that women who began hormone therapy within 10 years of menopause had a significantly lower risk of coronary heart disease compared to those who started later (or not at all).
Improved Sleep Quality
Many women experience sleep disturbances during menopause. HRT can help alleviate night sweats and hot flashes, which often disrupt sleep. A study in the journal Sleep Medicine Reviews reported that hormone therapy improved sleep quality in up to 65% of menopausal women (a finding that highlights the potential of HRT to enhance overall well-being through better rest).
While these benefits are promising, it’s important to note that HRT is not without risks. Each individual should consult with a healthcare provider to determine if hormone replacement therapy suits their specific situation. The next section will explore the potential risks and side effects associated with hormone therapy, providing a balanced view of this treatment option.
What Are the Risks of Bioidentical Hormones?
Bioidentical hormones offer potential benefits, but they also come with risks that patients should carefully consider. This chapter explores the potential downsides of bioidentical hormone therapy.
Cancer Risk Considerations
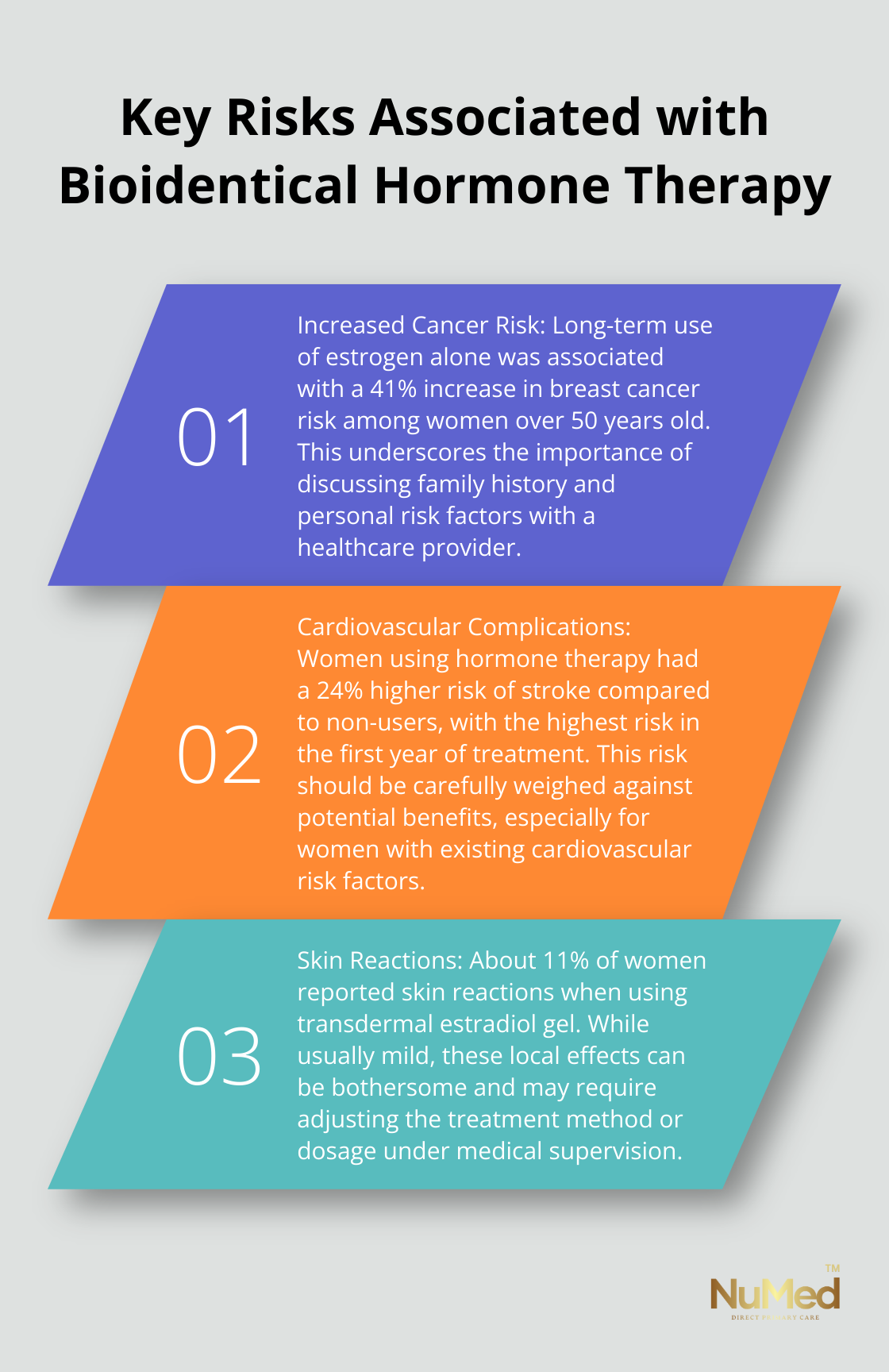
The relationship between hormone therapy and cancer risk is complex. The Nurses’ Health Study found a significant 41% increase in breast cancer risk among women over 50 years who used estrogen alone for long-term use. However, estrogen-only therapy in women who have had a hysterectomy showed a decreased risk of breast cancer.
Endometrial cancer risk is another concern. Women with an intact uterus who use estrogen alone have a significantly increased risk of endometrial cancer. This risk can be mitigated by adding progestin to the hormone therapy regimen.
Cardiovascular Complications
Blood clots and stroke are serious potential side effects of hormone therapy. Recent findings suggest that opting for transdermal estrogen over oral formulations may reduce the risk of VTE and its recurrence, offering a safer option for hormone therapy.
A large Danish study found that women using hormone therapy had a 24% higher risk of stroke compared to non-users. The risk was highest in the first year of treatment and decreased over time.
Skin Reactions and Local Effects
Topical hormone preparations can cause skin irritation, redness, or itching at the application site. In a study of transdermal estradiol gel, about 11% of women reported skin reactions. These effects are usually mild but can be bothersome for some patients.
Hormonal Imbalances and Mood Changes
Hormone therapy can sometimes lead to mood swings or depression, especially if the dosage isn’t properly balanced. A study in the journal Menopause found that about 6% of women using bioidentical hormone therapy reported mood swings as a side effect.
It’s important to work closely with a healthcare provider to monitor hormone levels and adjust treatment as needed. A personalized approach to hormone therapy (with regular assessment of patients’ responses and necessary adjustments) can help mitigate these risks.
Monitoring and Management
Regular check-ups and screenings are essential for anyone undergoing hormone therapy. The North American Menopause Society recommends annual breast examinations, mammograms, and pelvic exams for women using hormone therapy.
Blood tests to monitor hormone levels should be conducted periodically. These tests are typically performed every 3-6 months during the first year of treatment, then annually if the patient is stable.
Final Thoughts
Bioidentical hormones offer potential benefits and risks. The pros and cons of bioidentical hormones must be evaluated for each individual. Factors such as age, medical history, and specific symptoms influence the most appropriate treatment approach.
Personalized medical advice is essential when considering hormone therapy. Regular monitoring and adjustments maximize benefits while minimizing risks. Future research will likely focus on refining treatment protocols and exploring new delivery methods.
We at NuMed Direct Primary Care take a holistic approach to healthcare. Our comprehensive services can help you navigate complex health decisions like hormone therapy. The decision to use bioidentical hormones should be made in consultation with a qualified healthcare provider.