Direct Primary Care (DPC) has gained traction as an alternative healthcare model, but it’s not without its critics. At NuMed DPC, we believe in addressing these concerns head-on to provide a clearer picture of DPC’s role in modern healthcare.
This post will explore common Direct Primary Care criticisms, including coverage limitations, potential overutilization, and affordability issues. We’ll also discuss how DPC fits into the broader healthcare landscape and why we believe it’s a vital part of improving patient care and reducing costs.
Unpacking Direct Primary Care Criticisms
Direct Primary Care (DPC) faces several criticisms despite its growing popularity as an alternative healthcare model. This chapter examines the most common concerns raised about DPC and provides context for these issues.
Specialized Care Limitations
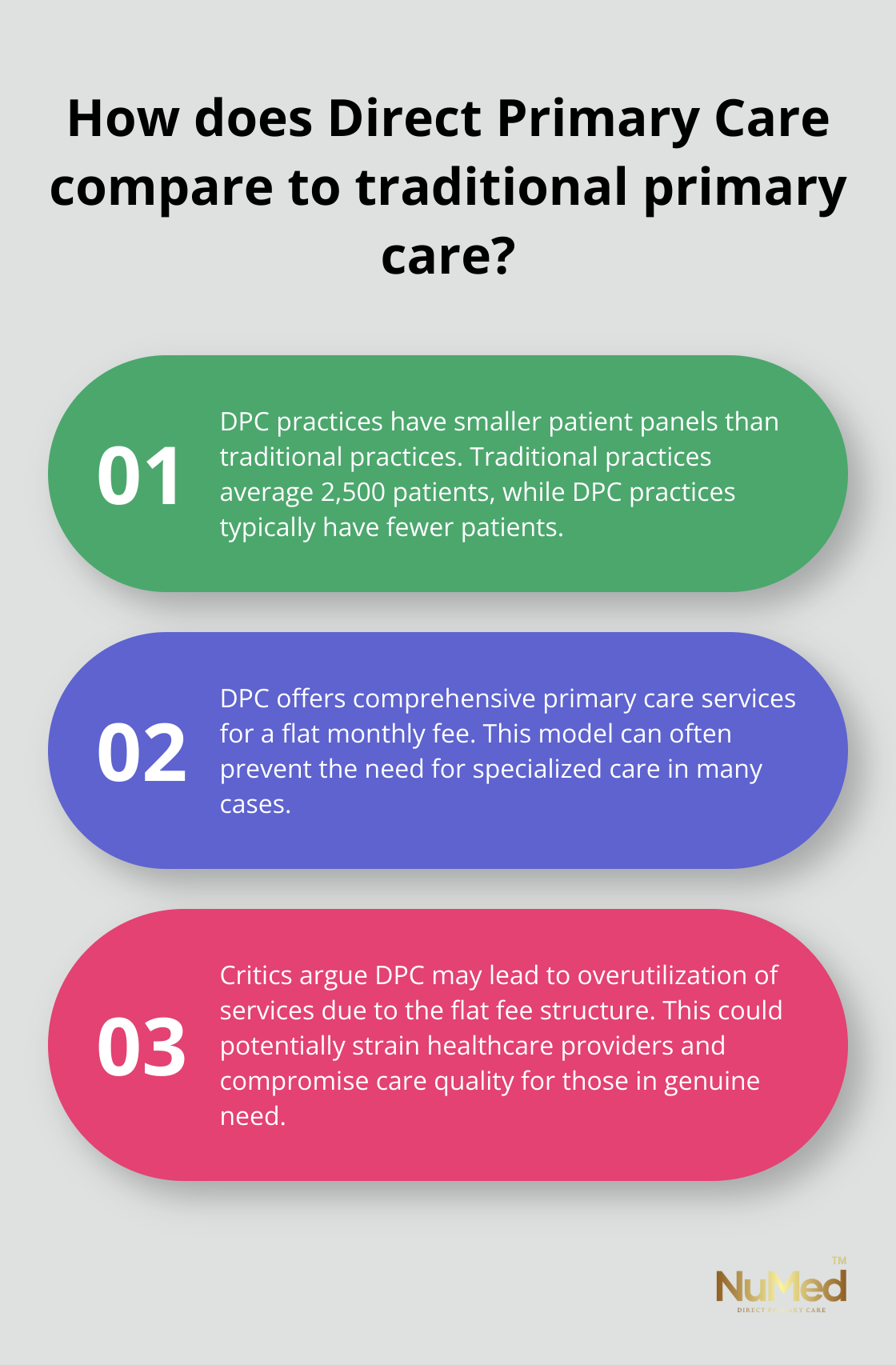
Critics often point to DPC’s limited coverage for specialized care. Patients might still need traditional insurance for services outside the scope of primary care, such as surgeries or cancer treatments. This observation holds merit – DPC does not aim to replace all forms of healthcare coverage. Instead, it provides comprehensive primary care services, which can often prevent the need for specialized care in many cases. It’s worth noting that traditional primary care practices have an average patient panel size of 2,500 patients, while DPC practices typically have smaller panel sizes, allowing for more personalized care.
Overutilization Concerns
Another criticism focuses on the potential overutilization of services. Some argue that because patients pay a flat fee, they might visit their doctor more frequently, even for minor issues. While increased access to care generally benefits patients, critics worry this could lead to unnecessary strain on healthcare providers and potentially compromise the quality of care for those who truly need it.
Affordability for Low-Income Patients
The most significant criticism of DPC centers on affordability for low-income patients. Critics argue that the monthly membership fees (while often lower than traditional insurance premiums) might still exceed the budgets of some individuals and families. This raises questions about DPC’s ability to address healthcare disparities and provide equitable access to care.
Critics believe that direct primary care is a solution for a limited group of people: the relatively healthy ones, those who can’t afford insurance and don’t qualify for subsidies. Many DPC practices strive to keep their fees as affordable as possible. Some practices even offer sliding scale fees based on income. However, the affordability concern remains a key point of discussion in the ongoing debate about DPC’s role in the broader healthcare landscape.
These criticisms highlight important considerations in the DPC model. As healthcare delivery continues to evolve, addressing these concerns will play a vital role in the long-term success and acceptance of Direct Primary Care. The next section will explore how DPC practices (including NuMed DPC) work to address these concerns and provide value to patients across various income levels.
Is DPC Really Affordable?
Comparing Costs: DPC vs. Traditional Insurance
Direct Primary Care (DPC) offers a cost-effective alternative to traditional healthcare models. A study published in the Journal of General Internal Medicine reveals that patients pay between $75 and $88 per month for DPC memberships (annual cost: $900 to $1,056). In contrast, the Kaiser Family Foundation reports that the average premium for patients in traditional fee-for-service models is $1,400 yearly, with only about 6% allocated for primary care.
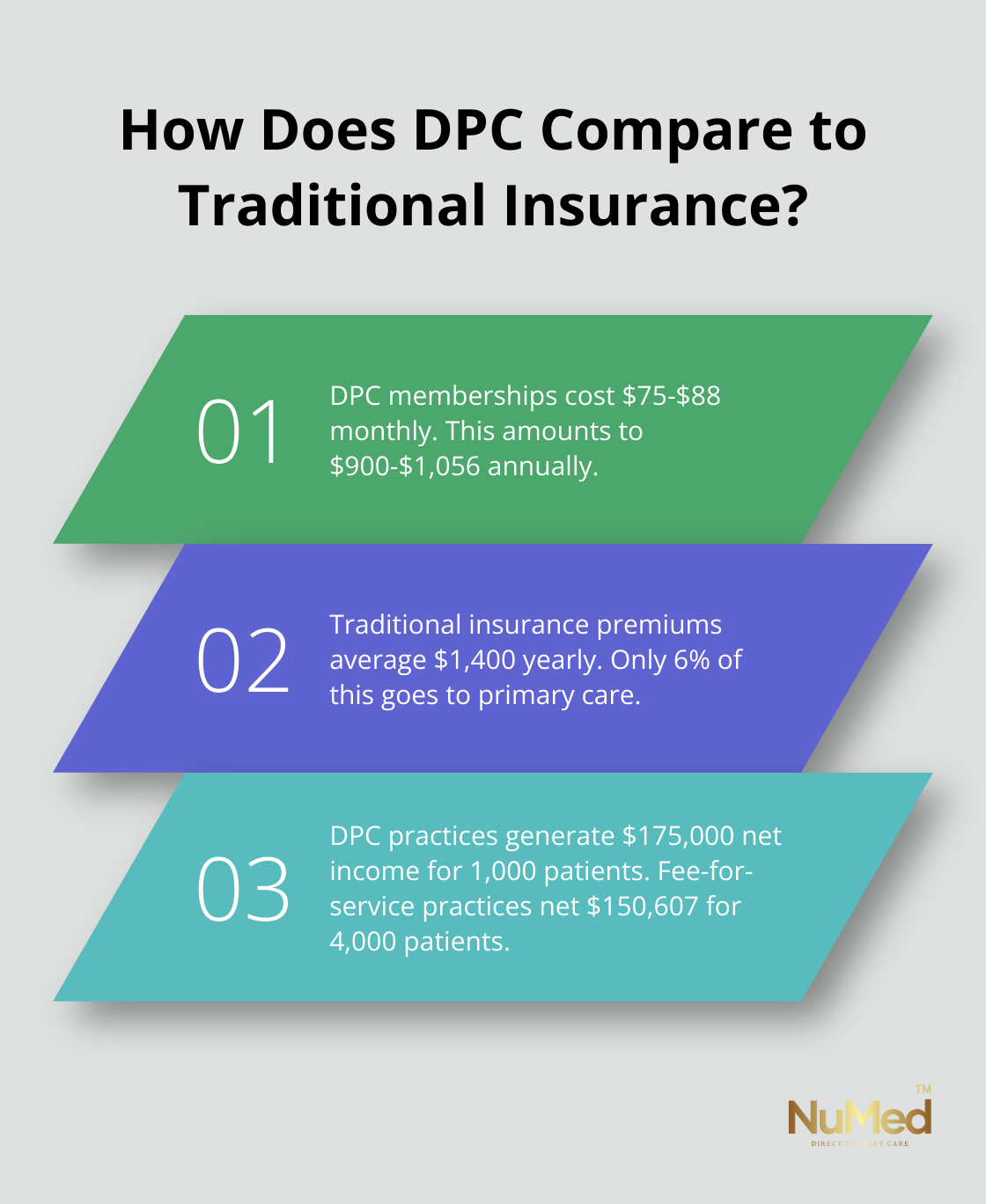
Patients with chronic conditions requiring frequent care often experience significant savings with DPC. A recent analysis demonstrated that DPC practices generate a net income of $175,000 yearly for 1,000 patients, while a typical fee-for-service practice nets $150,607 for 4,000 patients. This efficiency allows DPC practices to provide more personalized care at a lower cost.
The Transparency Factor
DPC’s appeal lies in its transparent pricing and services. Unlike traditional healthcare models (which often involve complex billing systems and hidden fees), DPC practices typically offer a clear, all-inclusive fee structure. This transparency empowers patients to budget their healthcare expenses more effectively, without the fear of unexpected costs.
Many DPC practices provide a comprehensive list of services covered under their membership fee. This often includes unlimited office visits, telemedicine consultations, and even some basic lab work. Patients can make informed decisions about their healthcare spending when they know exactly what they’re paying for.
Prevention: The Financial Game-Changer
The DPC model’s focus on preventive care leads to significant long-term cost savings. DPC practices try to prevent or manage chronic conditions before they become more serious (and expensive) to treat by emphasizing early intervention and lifestyle changes.
A study published in the American Journal of Managed Care found that patients in DPC practices had 25.5% lower hospital admissions compared to traditional practices. Emergency room visits also decreased by 53.6%. These reductions in high-cost interventions translate to substantial savings for both patients and the healthcare system as a whole.
Affordability for Different Demographics
While DPC may not be the cheapest option for every individual, its combination of transparent pricing, comprehensive primary care, and focus on prevention makes it a financially viable and potentially cost-saving option for many patients. Some DPC practices (including top choices like NuMed DPC) offer sliding scale fees based on income, making the model more accessible to a wider range of patients.
As we explore the role of DPC in the broader healthcare system, it’s important to consider how this model complements traditional insurance and contributes to overall healthcare cost reduction.
How DPC Fits Into the Healthcare Landscape
Complementing Catastrophic Coverage
Direct Primary Care (DPC) serves as a vital component in the evolving healthcare ecosystem. DPC practices work alongside traditional insurance models to provide comprehensive care while addressing systemic issues in the healthcare industry.
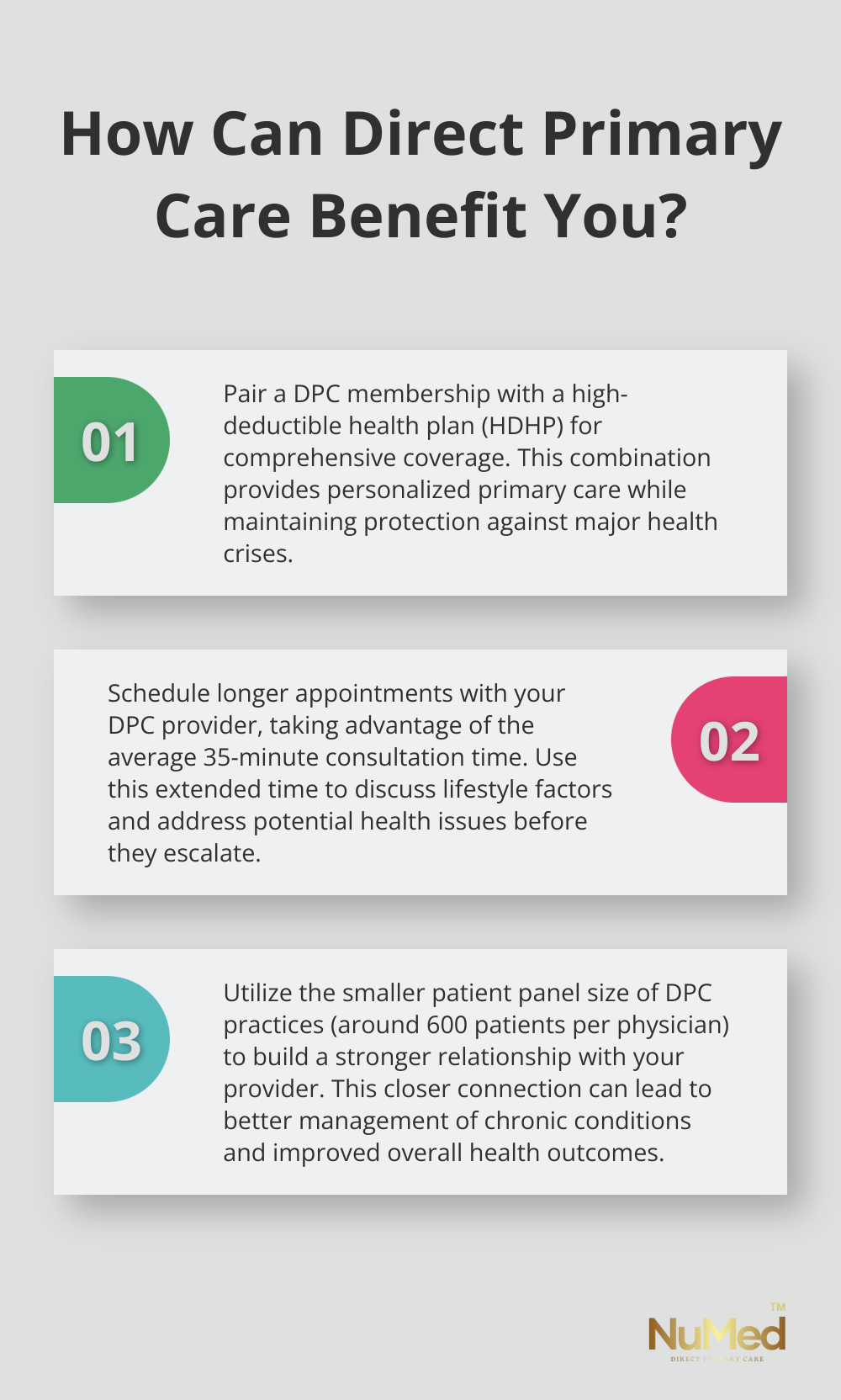
DPC memberships cover a wide range of primary care services but don’t replace the need for catastrophic coverage. Many DPC patients pair their membership with a high-deductible health plan (HDHP) for major medical events. This combination allows patients to benefit from personalized primary care while maintaining protection against significant health crises.
A study found that HDHPs typically have lower premiums but greater member cost-sharing than traditional health plans. From 2021, HDHPs have always had lower out-of-pocket costs for members compared to traditional insurance plans. This reduction in costs indicates that the preventive focus of DPC can lead to fewer major health events requiring expensive interventions.
Cost Reduction Through Prevention
DPC’s emphasis on prevention and early intervention changes the game for healthcare costs. A study reported that DPC patients had fewer ER visits compared to those in traditional practices. These reductions translate to significant cost savings for both patients and the healthcare system as a whole.
DPC practices achieve these results through longer appointment times, which allow for more thorough examinations and discussions about lifestyle factors. The average DPC appointment lasts 35 minutes (compared to just 18 minutes in traditional primary care settings). This extra time enables practitioners to address potential health issues before they escalate into costly problems.
Improved Patient Satisfaction and Outcomes
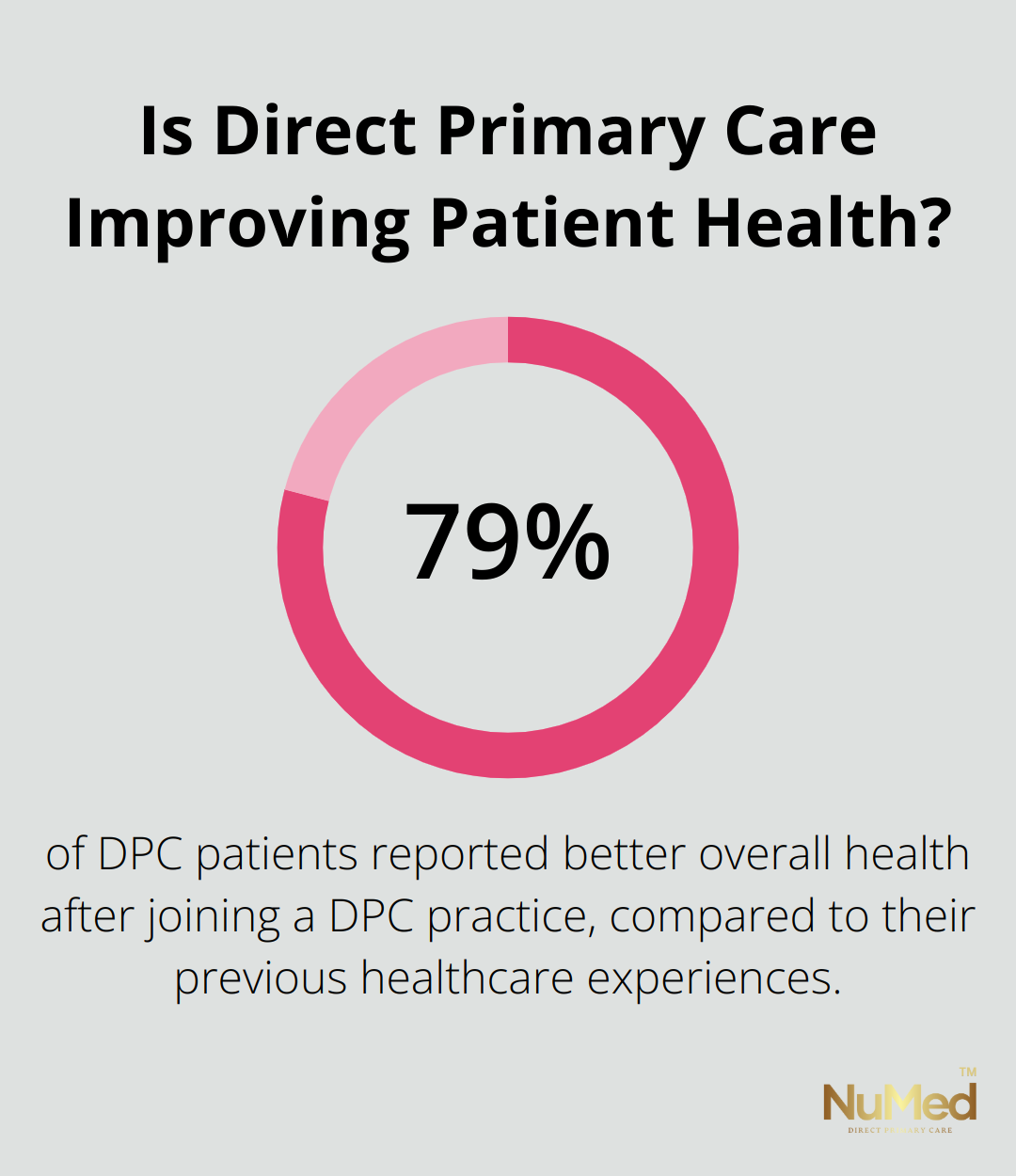
The DPC model’s focus on building strong patient-provider relationships leads to improved health outcomes and higher satisfaction rates. A survey conducted by the Direct Primary Care Coalition found that 79% of DPC patients reported better overall health after joining a DPC practice, compared to their previous healthcare experiences.
DPC practices typically maintain smaller patient panels, averaging around 600 patients per physician (compared to 2,500 in traditional practices). This reduced patient load allows for more personalized care and better continuity, which are crucial factors in managing chronic conditions and preventing complications.
The healthcare landscape continues to evolve, and DPC plays a significant role in shaping a more patient-centered, cost-effective system. DPC addresses many of the challenges facing modern healthcare delivery by complementing traditional insurance, focusing on prevention, and improving patient outcomes.
Final Thoughts
Direct Primary Care (DPC) represents a significant shift in healthcare delivery, offering numerous benefits while addressing longstanding issues in traditional models. DPC criticism often centers on specialized care limitations, potential overutilization, and affordability concerns. However, these critiques must be balanced against the model’s strengths in prevention, personalized care, and transparent pricing.
DPC plays an increasingly important role in healthcare reform as patients seek more personalized, accessible care options. The model’s ability to complement high-deductible health plans provides a pathway for comprehensive coverage while controlling costs. DPC practices like NuMed Primary Care address common criticisms head-on by combining the best aspects of DPC with functional medicine and health coaching.
NuMed DPC’s transparent pricing structure and absence of insurance hassles make healthcare more accessible and understandable for patients. We foster long-term relationships and provide readily available support to improve both physical and emotional health outcomes. Our model demonstrates that DPC can effectively balance affordability with high-quality, personalized care.