Traditional healthcare often treats symptoms after diseases develop. Lifestyle medicine takes a different approach by addressing the root causes of chronic conditions through evidence-based interventions.
We at NuMed DPC integrate lifestyle medicine into our direct primary care model, giving patients the time and personalized attention needed for lasting health changes. This comprehensive approach transforms how people prevent and manage chronic diseases.
How Does Lifestyle Medicine Work in DPC
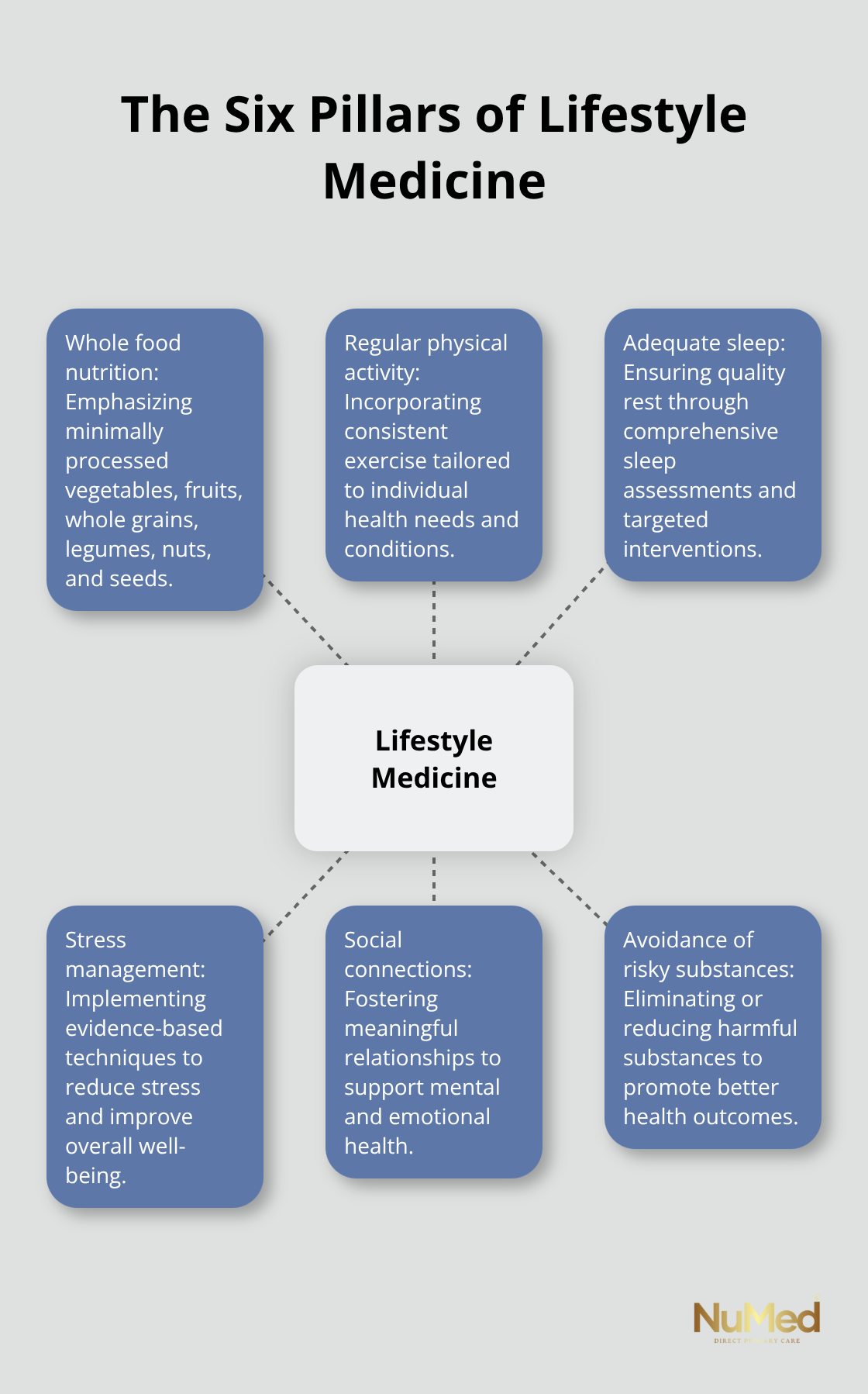
The Six Pillars Framework
Lifestyle medicine operates on six evidence-based pillars that address the root causes of chronic disease. These pillars include whole food nutrition, regular physical activity, adequate sleep, stress management, social connections, and avoidance of risky substances. The American College of Lifestyle Medicine reports that poor diet quality remains the leading cause of premature death in America, which makes these interventions medical necessities rather than wellness trends.
DPC practices provide the ideal environment for the implementation of these pillars because physicians can spend 30 to 60 minutes per visit instead of the typical 7-minute appointments in traditional healthcare. This extended time allows for comprehensive assessment of lifestyle factors, detailed education on behavior change, and continuous support for sustainable modifications. Research shows that meaningful lifestyle interventions require consistent follow-up and personalized guidance (which traditional healthcare models cannot provide due to time constraints and reimbursement limitations).
Comprehensive Care Integration
DPC models excel at lifestyle medicine because they eliminate the barriers that prevent effective implementation in traditional healthcare settings. Without insurance restrictions, physicians can focus on preventive interventions that address underlying causes rather than manage symptoms. Studies indicate that approximately 60% of Americans have at least one chronic disease, with healthcare costs that reach $4.9 trillion annually. Most of these conditions stem from lifestyle factors that respond well to targeted interventions when patients receive adequate support and education.
The monthly membership model allows for unlimited visits, phone consultations, and email communication, which creates multiple touchpoints for lifestyle coaching and accountability. This continuous engagement proves essential for behavior change, as patients typically need 3-6 months of consistent support to establish new habits that become permanent lifestyle modifications.
Evidence-Based Treatment Protocols
Physicians in DPC settings can implement comprehensive lifestyle medicine protocols that traditional practices cannot accommodate. They conduct detailed nutritional assessments, create personalized exercise prescriptions, and develop stress management strategies tailored to each patient’s specific needs. The American College of Lifestyle Medicine advocates for diets rich in minimally processed vegetables, fruits, whole grains, legumes, nuts, and seeds to improve health outcomes (particularly for patients with cardiovascular disease and type 2 diabetes).
These evidence-based interventions require time for proper implementation and patient education. DPC physicians can spend adequate time to explain the science behind lifestyle recommendations, address patient concerns, and modify treatment plans based on individual responses and preferences.
What Specific Interventions Transform Health in DPC
Personalized Nutrition Strategies That Work
DPC physicians create detailed nutritional assessments that go far beyond basic dietary advice. They analyze patient food logs, conduct micronutrient tests, and identify specific inflammatory triggers that contribute to chronic conditions. The American College of Lifestyle Medicine emphasizes that whole food plant-based diets can effectively cure and control diabetes, eliminating medicine or insulin requirements when physicians implement them with consistent monitoring.
Physicians develop meal plans that address individual metabolic profiles, food sensitivities, and cultural preferences. Patients receive weekly check-ins during the first month, then biweekly follow-ups to adjust macronutrient ratios based on lab results and symptom improvements. This intensive approach produces measurable results because patients get immediate feedback and course corrections rather than waiting months between appointments.
Exercise Prescriptions Based on Medical Data
DPC practices prescribe exercise like medication with specific dosages, frequencies, and progressions tailored to each patient’s health status. Adults need 150 minutes of moderate aerobic activity weekly according to CDC guidelines, but patients with cardiovascular disease require different intensities and monitoring protocols than those with arthritis or diabetes.
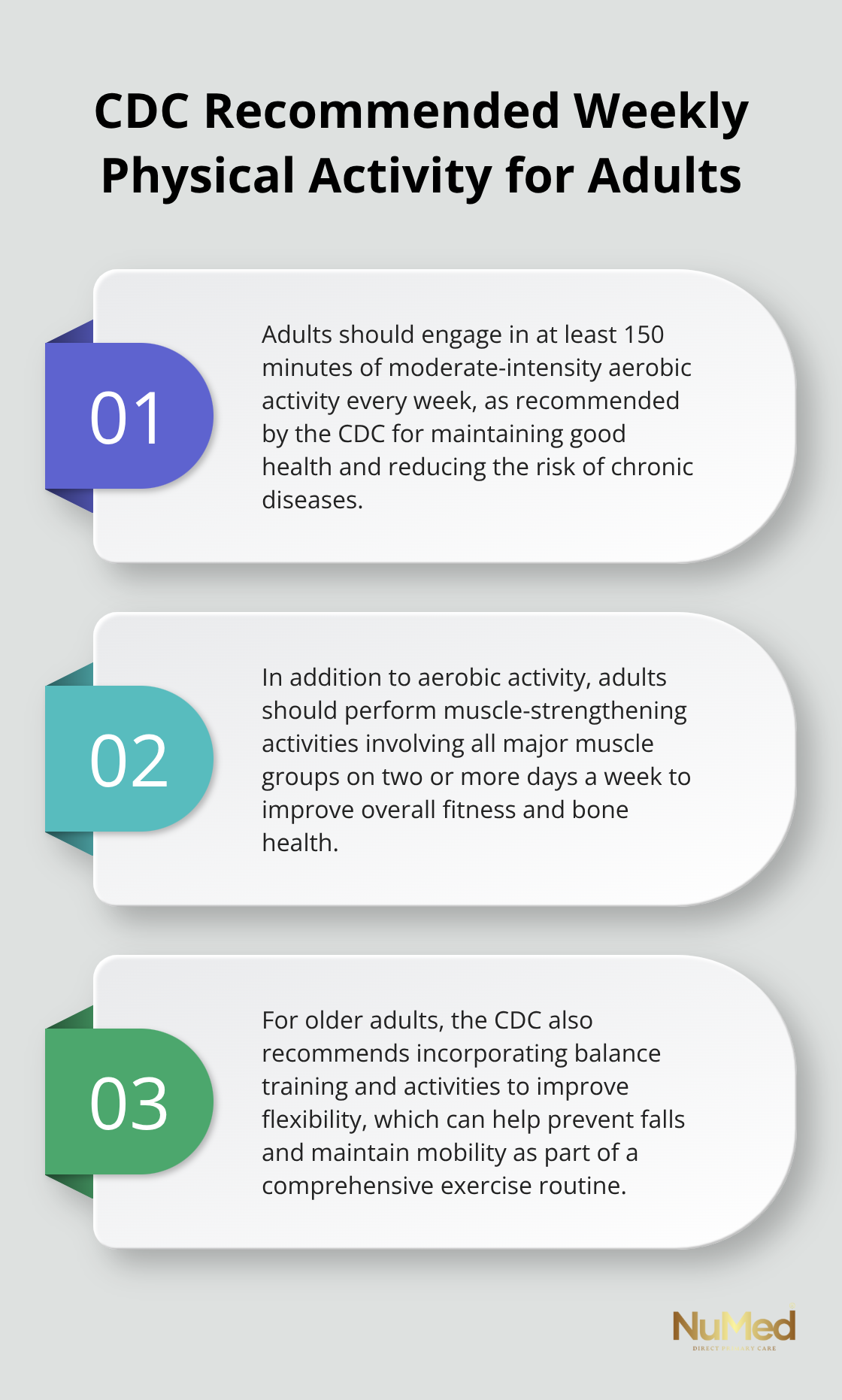
Physicians conduct baseline fitness assessments, review cardiac stress tests when necessary, and create progressive movement plans that start with patient capabilities rather than generic recommendations. They track heart rate variability, blood pressure responses, and inflammatory markers to adjust exercise prescriptions monthly. This medical approach to fitness prevents injuries and maximizes therapeutic benefits because each prescription addresses specific health conditions rather than general wellness goals.
Sleep and Stress Interventions With Measurable Outcomes
Quality sleep and stress management require medical intervention rather than lifestyle suggestions. DPC physicians conduct comprehensive sleep assessments (including sleep studies when indicated), hormone tests to identify cortisol dysregulation, and heart rate variability monitoring to track autonomic nervous system function.
They prescribe specific sleep hygiene protocols, recommend targeted supplements like magnesium glycinate for patients with documented deficiencies, and teach evidence-based stress reduction techniques such as heart rate variability training. Patients receive sleep tracking devices and weekly data reviews to identify patterns and adjust interventions. This systematic approach addresses the root causes of sleep disorders and chronic stress rather than masking symptoms with medications.
These targeted interventions work because DPC physicians can monitor progress closely and adjust treatments based on real-time data. The comprehensive nature of lifestyle medicine in DPC settings creates synergistic effects that amplify health improvements across multiple body systems.
What Real Results Does Lifestyle Medicine Deliver in DPC
Disease Prevention Through Root Cause Treatment
DPC practices prevent chronic diseases by targeting root causes rather than managing symptoms after conditions develop. Patients with diabetes who receive comprehensive lifestyle interventions through DPC show significant improvements in blood sugar control compared to traditional care models. The American Academy of Family Physicians reports that DPC patients experience 40% fewer emergency room visits because physicians address health issues before they escalate into crises.
This proactive approach works because DPC physicians can spend adequate time to identify inflammatory triggers, metabolic dysfunction, and behavioral patterns that traditional healthcare models miss due to time constraints. Physicians detect early warning signs through monthly biomarker tests and adjust treatment protocols immediately rather than wait for annual check-ups when conditions have already progressed.
Financial Impact of Prevention-Based Care
DPC memberships cost $50 to $100 monthly but generate significant savings through disease prevention and early intervention. Families who utilize DPC achieve a 20-30% reduction in overall healthcare costs by avoiding emergency visits and reducing specialist referrals. The Centers for Disease Control and Prevention calculates that chronic diseases contribute $4.9 trillion annually to healthcare spending (with most conditions preventable through lifestyle modifications).
DPC patients receive discounted lab tests and imaging because physicians negotiate pricing directly with providers. This eliminates insurance markup costs that inflate traditional healthcare expenses. Patients avoid copays, deductibles, and surprise billing that plague traditional healthcare models.
Measurable Health Transformations
DPC patients achieve superior health outcomes through consistent monitoring and personalized interventions that traditional practices cannot provide. A Primary Care Collaborative survey showed that 93% of DPC patients reported improved management of chronic conditions, resulting in fewer sick days and better quality of life.
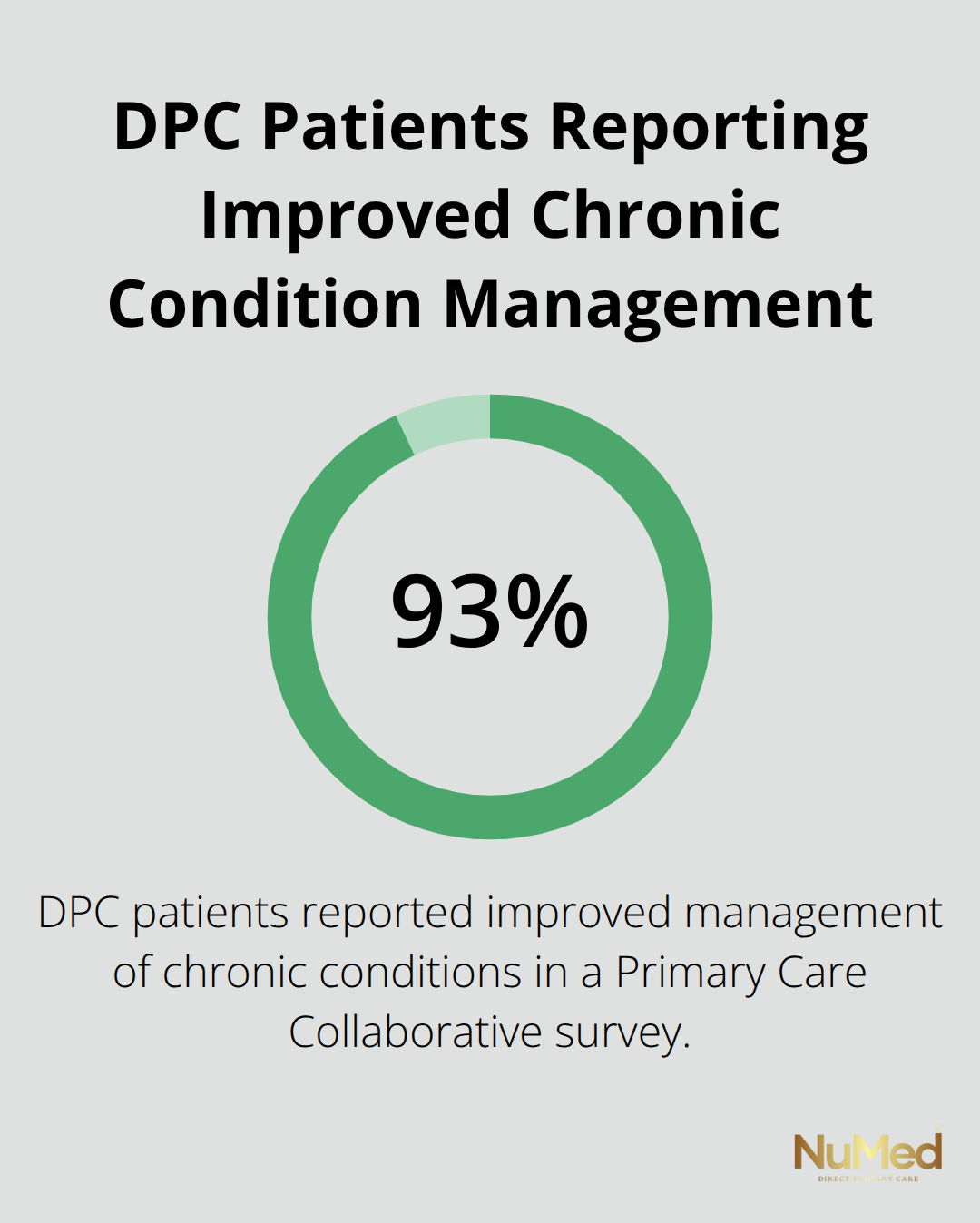
This intensive approach produces measurable results because patients receive continuous feedback and course corrections based on real-time data rather than waiting months between appointments for generic recommendations. Patients see improvements in inflammatory markers, blood pressure readings, and metabolic function within 90 days of starting comprehensive lifestyle interventions through DPC practices.
Final Thoughts
Lifestyle medicine transforms health when physicians address root causes rather than symptoms. This approach creates lasting changes that prevent chronic diseases and reduce healthcare costs. The evidence demonstrates that comprehensive interventions produce measurable improvements in patient outcomes when doctors implement them with adequate time and personalized attention.
DPC provides the optimal framework for lifestyle medicine because physicians spend 30-60 minutes per visit and offer unlimited consultations. This intensive approach generates superior results compared to traditional healthcare models that lack time for proper implementation of evidence-based interventions. The monthly membership model eliminates insurance barriers that prevent effective lifestyle medicine delivery in conventional practices.
Patients receive immediate access to comprehensive assessments, personalized treatment protocols, and ongoing support that creates sustainable behavior changes. This proactive approach prevents disease progression and reduces long-term healthcare expenses. NuMed DPC combines lifestyle medicine with direct primary care to deliver compassionate healthcare that addresses root causes through personalized treatment plans (with transparent pricing and accessible support that helps patients achieve optimal health outcomes).